|
Abstract:
Congenital anomalies of the gallbladder, such as
the bilobed gallbladder (vesica fellea
divisa), are rare clinical entities with
an estimated incidence of 1 in 4,000 live
births. These variations pose significant
intraoperative challenges, particularly when
compounded by a "frozen abdomen" from previous
surgical interventions. We report a unique case
of a 30-year-old male with a history of open
surgery for hepatic hydatid disease who
presented with recurrent right hypochondrium
pain and vomiting. Preoperative imaging
identified a large splenic hydatid cyst and
cholelithiasis. While the splenic cyst was
managed laparoscopically after insertion of the
first trocar via Palmer’s point to avoid
suspected adhesions, the gallbladder surgery
required conversion to an open approach due to
dense, matted adhesions at the gallbladder bed.
Intraoperatively, a rare vesica fellea
divisa (Boyden’s type) was discovered,
containing multiple calculi in both lobes but
draining into a single cystic duct. A total
cholecystectomy was successfully performed.
Histopathological examination confirmed a
splenic hydatid cyst and chronic cholecystitis
with no evidence of malignancy. The patient
remained asymptomatic and expressed high
satisfaction at his six-month follow-up. This
case underscores the rarity of splenic
hydatidosis and the critical need for surgical
flexibility and meticulous anatomical
delineation when encountering unexpected
congenital biliary anomalies in a re-operative
surgical field.
Key
Words: Bilobed gallbladder, Splenic
hydatid cyst, Boyden's classification, Frozen
abdomen, Cholecystectomy, Vesica fellea divisa.
|
|
Introduction
The
gallbladder is known for a wide range of
congenital anatomical variations, which often pose
significant challenges during surgical
interventions. Among these, the duplicated
gallbladder is an exceedingly rare anomaly with an
estimated incidence of approximately 1 in 4,000
live births [1, 2]. They are often asymptomatic
but can become clinically significant when
complicated by cholelithiasis or when they coexist
with other pathologies. Surgeons need to be aware
of this congenital abnormality due to its
association with anatomical variations of the
hepatic artery and cystic duct. There are two
classification systems for duplicated gallbladder,
namely Boyden's classification and Harlaftis
classification [3]. Boyden's classification is
more widely accepted due to its simplicity, and it
describes two main types:
- Vesica fellea divisa: wherein
there is a bilobed gallbladder draining into a
single cystic duct,
- Vesica fellea duplex: wherein
gallbladder is truly duplicated and draining
into separate cystic ducts. This type is
sub-classified into the “Y-shaped type” (two
cystic ducts uniting and then entering the
common bile duct), and the “H-shaped or ductular
type” (two cystic ducts entering separately into
the common bile duct).
Hydatid disease,
caused by Echinococcus species, remains
a significant public health concern in endemic
regions. While the liver is the most common site
of infection (70%), splenic hydatid cysts are
rare, accounting for only up to 5% of all cases
[4]. This rarity is attributed to the "filtering"
action of the liver and lungs, which act as the
first and second barriers to the systemic
circulation of embryos.
The simultaneous
clinical presentation of a symptomatic splenic
hydatid cyst and a congenital vesica fellea divisa
represents an exceptionally rare surgical
intersection. We herein present one such case to
highlight the diagnostic challenges and technical
nuances required to manage such concurrent
pathologies in the presence of a frozen abdomen.
Case Presentation
A 30-year-old male
presented with a one-year history of recurrent
vomiting and pain in the right hypochondrium
(RHC). His past medical history was significant
for an open surgical intervention for hepatic
hydatid disease performed three years prior.
Ultrasonography (USG) suggested the presence of a
splenic cyst and cholelithiasis. A subsequent
Computed Tomography (CT) scan confirmed a large
cystic lesion in the spleen, characteristic of a
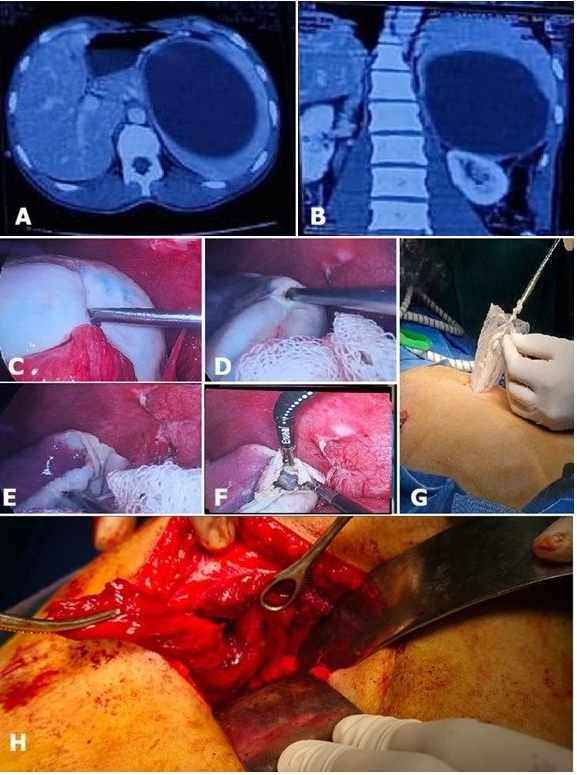
Gharbi Type 1 - hydatid cyst (Figure 1 A, B),
alongside a distended gallbladder containing
multiple calculi. The splenic cyst measured
approximately 12 x 10 x 9 cm with an estimated
volume of about 550 mL. Serological testing,
specifically Enzyme-Linked Immunosorbent Assay
(ELISA) and Indirect Hemagglutination (IHA) for Echinococcus
antibodies, returned positive results, providing
immunological confirmation of hydatid disease.
The procedure began
with a diagnostic laparoscopy. To avoid suspected
dense adhesions from the previous hepatic surgery,
access was gained via Palmer’s point. The splenic
hydatid cyst was successfully managed using a
laparoscopic approach (Figure 1 C-G). However,
upon exploration of the right hypochondrium,
"frozen" anatomy was encountered. Dense, matted
adhesions involving the omentum, colon, stomach,
and duodenum were found at the gallbladder bed,
resulting from the previous open hepatic surgery.
Due to the inability to safely visualize Calot’s
triangle, the team converted to an open approach
via a right subcostal incision over the old scar.
Following extensive
adhesiolysis, a congenital anomaly was discovered:
a bilobed gallbladder (vesica fellea divisa). Both
lobes were filled with multiple calculi.
Meticulous dissection revealed that both lobes
drained into a single cystic duct and were
supplied by a single cystic artery (Figure 1 H). A
total cholecystectomy was successfully performed.
Histopathological
examination confirmed the diagnosis of a hydatid
cyst of the spleen and revealed features of
chronic cholecystitis in the gallbladder specimen,
with no evidence of malignancy in either lobe. The
patient's postoperative recovery was uneventful.
At the six-month follow-up, the patient reported
complete resolution of symptoms and expressed high
satisfaction with the surgical outcome.
|
| Figure
1: Radiological and Intraoperative
Findings. (A, B)
Axial and coronal sections of the abdominal
computed tomography (CT) scan demonstrating
a large, unilocular splenic hydatid cyst. (C–G)
Sequential intraoperative steps showing the
laparoscopic evacuation and management of
the splenic hydatid cyst. (H)
Intraoperative view after conversion to open
surgery, showing the two distinct lobes of
the bilobed gallbladder (vesica fellea
divisa) held with surgical
instruments for anatomical delineation. |
Discussion
The discovery of a
bilobed gallbladder intraoperatively is a rare
event that demands meticulous surgical technique
to ensure the "critical view of safety" and
prevent iatrogenic injury. Based on the Boyden
classification, our case fits the description of vesica
fellea divisa. In this subtype, the
gallbladder primordium divides during the 5th or
6th week of gestation, resulting in two lobes that
communicate through a single cystic duct [3].
In this patient, the
surgical complexity was significantly increased by
a prior open hepatic hydatid surgery. Previous
interventions for hydatid disease are often
associated with dense, "matted" adhesions
involving the omentum, stomach, and duodenum,
leading to what is clinically described as a
frozen abdomen [5]. While the splenic hydatid cyst
was successfully managed laparoscopically via
Palmer’s point to avoid adhesions, the gallbladder
pathology necessitated conversion to an open
approach. Literature suggests that conversion
rates are higher in patients with previous upper
abdominal surgeries due to the high risk of
visceral injury during laparoscopic dissection of
the Calot’s triangle [6].
The presence of
multiple gallbladders or lobes does not
necessarily increase the risk of cholelithiasis;
however, if stones are present, they usually
affect both lobes, as seen in our patient. It is
imperative for the surgeon to excise both lobes
entirely to prevent "stump cholecystitis" or
recurrent symptoms from a residual lobe [7].
This case highlights
the importance of maintaining a high index of
suspicion for anatomical variations even when
preoperative imaging is inconclusive. The
successful management of a rare splenic hydatid
cyst alongside a congenital biliary anomaly
underscores the need for surgical flexibility and
careful intraoperative anatomical delineation.
Conclusion
This case emphasizes
the necessity of surgical flexibility when
managing rare congenital and infective pathologies
in a re-operative field. The presence of a "frozen
abdomen" often necessitates a low threshold for
conversion from laparoscopy to an open approach to
ensure the safe visualization of anatomical
landmarks. Intraoperatively, the discovery of a vesica
fellea divisa demands meticulous dissection
to identify the single cystic duct and artery.
Ultimately, thorough intraoperative evaluation and
complete resection of all gallbladder lobes are
paramount to preventing recurrent symptoms and
ensuring successful surgical outcomes.
Informed Consent
Written informed consent was obtained from the
patient for the publication of this case report
and any accompanying images.
Acknowledgments
The authors would like to express their sincere
gratitude to the patient for his cooperation and
for providing consent to share this clinical
finding with the medical community.
References
- Kumar M, Adhikari D, Kumar V, Dharap S.
Bilobed gallbladder: a rare congenital anomaly.
BMJ Case Rep. 2018 Feb 11;2018:
bcr2017222783. doi: 10.1136/bcr-2017-222783.
- Pillay Y. Gallbladder duplication. Int J
Surg Case Rep 2015; 11:18–20.
10.1016/j.ijscr.2015.04.002
- Robele TK, Mulugeta S, Knfe G, Dagne D,
Shiferaw E. Duplicated gallbladder with stones:
Rare anomaly of the biliary system. Int J
Surg Case Rep. 2024 Sep; 122:110106. doi:
10.1016/j.ijscr.2024.110106.
- Rasheed K, Zargar SA, Telwani AA. Hydatid cyst
of spleen: a diagnostic challenge. N Am J
Med Sci. 2013 Jan;5(1):10-20. doi:
10.4103/1947-2714.106184.
- Gómez Pérez JM, García Fernández GA, Lizárraga
Castro JA, Gómez Pérez AP, López Castillo R,
Hernández Álvarez CR. A review for hostile and
frozen abdomen. Int J Med Sci Clin Res Stud.
2024;4(9):1652–1654.
doi:10.47191/ijmscrs/v4-i09-10.
- Abraham S, Nemeth T, Benko R, et al.
Evaluation of the conversion rate as it relates
to preoperative risk factors and surgeon
experience: a retrospective study of 4013
patients undergoing elective laparoscopic
cholecystectomy. BMC Surg. 2021;21:151.
doi:10.1186/s12893-021-01152-z.
- Gigot J, Van Beers B, Goncette L, Etienne J,
Collard A, Jadoul P, Therasse A, Otte JB,
Kestens P. Laparoscopic treatment of gallbladder
duplication. A plea for removal of both
gallbladders. Surg Endosc. 1997
May;11(5):479-82. doi: 10.1007/s004649900396.
|



















