|
Introduction
Brown
tumour (BT) is a benign bony lesion caused by
rapid osteoclastic turnover of bone which is
localised, resulting from direct effects of
increased parathyroid hormone (PTH) seen in
primary hyperparathyroidism (PHPTH) or secondary/
tertiary hyperparathyroidism (SHPTH/ THPTH). BT
have been reported to occur in 2-3% patients of
HPTH, hence rarely seen in clinical practice [1].
Clinically, BT can present with pain in the bones
renal stones abdominal groans along with
psychiatric manifestations [2]. About 70% to 80%
of cases present asymptomatically and get
incidentally picked up while screening of calcium,
phosphate levels during other investigations In
contrast, advancements in biochemical screening
and increased clinical awareness have enabled the
early detection of PHPT, often in asymptomatic
individuals. Nonetheless, normocalcemic
hyperparathyroidism may represent an incipient
form of the disease [3]. The diagnosis of BT
requires a high index of suspicion as it is based
on a battery of tests from medical history,
clinical examination, laboratory results to
radiological imaging, where surgical biopsy and
histopathological evaluation are definitive for
diagnosis [4]. We present here, two cases with the
rare and first presentation of pathological
fractures and with histopathological diagnosis of
BT being crucial for the final work up leading
towards the diagnosis of PHPTH due to parathyroid
adenoma in both the cases.
Case Presentation
Case 1
A 43 year old male
presented with a left femur fracture, with history
of right tibia fracture four months back. He
complained of generalized fatigue and bony pains.
Body Bone scan was advised which revealed
multifocal involvement and suggested the diagnosis
of Metabolic bone disease possibly Multifocal low
grade infective/ inflammatory pathology. Few
excised bony tissue bits after open reduction and
internal fixation with intramedullary femur
nailing, showed multiple yellow brown soft to firm
tissue pieces altogether measuring 2x2x1cm were
sent for histopathological examination.
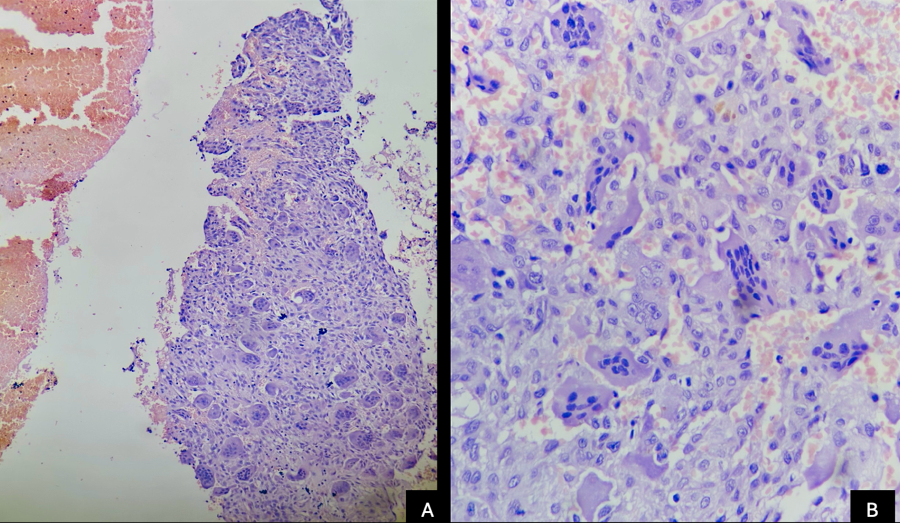
Microscopic examination revealed groups and
clusters of multinucleated osteoclastic giant
cells along with cells having oval to spindle
bland nuclei with indistinct cells borders and
eosinophilic cytoplasm. Viable and necrotic bony
trabeculae with intervening areas showing
trilineage haematopoiesis seen [Figure 1]. Thin
and thick walled blood vessels and hemosiderin
deposition also seen along with large areas of
haemorrhage.
|
| Figure
1: A - Low power view photomicrograph
showing giant cell clusters with
surrounding prominent foci of haemorrhage.
(H&E, 10X). B - High power view
photomicrograph showing sheets of
mononuclear cells admixed with
multinucleated osteoclastic giant cells.
Haematoxylin and eosin stain (H&E,
40X) |
Case 2
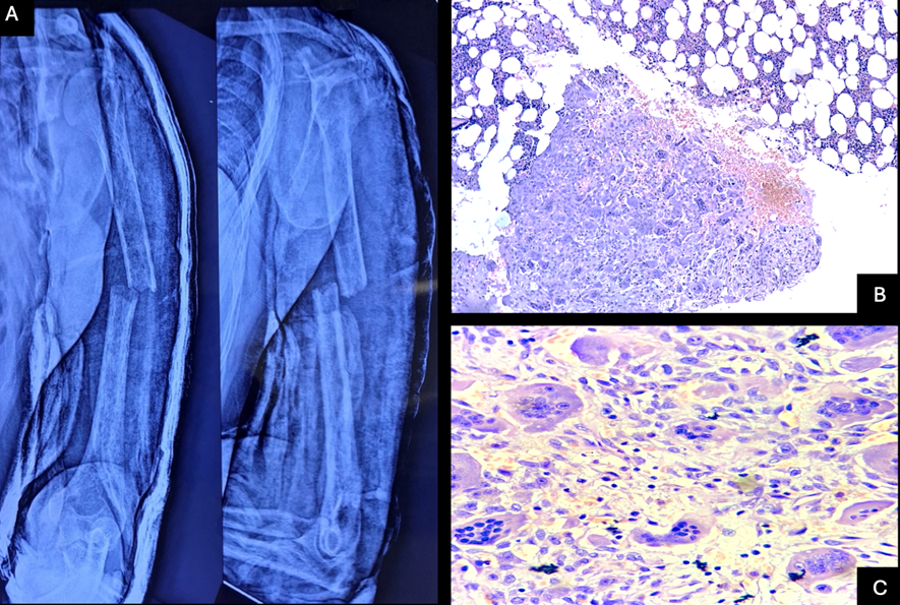
A 36 year old male presented with pain and
deformity at the site of five month old fracture
site, left humerus. X ray revealed decreased bone
density. Multiple grey brown soft to firm tissue
bits from intramedullary bone of fracture site,
altogether measuring 1.5x1.5x0.2cm was received
for histopathological examination, foci of
fibroblastic proliferation along with foamy
histiocytes, occasional multinucleated giant cells
and scattered hemosiderin laden macrophages were
seen along with enmeshed bony trabeculae and
unremarkable hematopoietic elements [Figure 2].
|
| Figure
2: A - Pathological fracture of the left
humerus in Case 2. B- Low power view
photomicrograph intervening areas of
trabeculae showing trilineage
haematopoiesis and areas of haemorrhage.
Haematoxylin and eosin stain (H & E,
10X). C - High power view photomicrograph
showing groups and clusters of
multinucleated osteoclastic giant cells
(arrow) along with cells having oval to
spindle bland nuclei with indistinct cells
borders and eosinophilic cytoplasm.
Histiocytes and hemosiderin laden
macrophages also seen. Haematoxylin and
eosin stain (H & E, 40X) |
Histopathological
diagnosis in Case 1 was BT and further work up was
advised. On work up the patient had markedly
raised PTH > 2500pg/mL and phosphorus levels
were low at 1.9mg/dL and. A clinical diagnosis of
hyperparathyroidism was made, thereafter a
Sestamibi scan was also performed and presence of
left inferior parathyroid adenoma was identified.
Similarly, histopathological features in Case 2
were suggestive of BT and laboratory and
radiological correlation was advised. Patient was
advised Sestamibi scan for parathyroid adenoma
localization based on the histopathological
diagnosis of BT and on scan inferior parathyroid
region shows an enlarged homogenous hypoechoic
lobulated mass 6 x 2.1 x 1.4 cm with peripheral
vascularity, suggestive of Right Inferior
Parathyroid Adenoma. Ultrasonography was also
suggestive of right parathyroid adenoma. Patient’s
calcium level was 13.4mg/dL with elevated PTH
>2500pg/mL. Both patients recovered after
orthopaedic procedures. They both underwent
parathyroidectomy. Recovery after surgery which
was uneventful with normal values of serum PTH and
calcium levels.
Discussion
Von Recklinghausen
termed osteitis fibrosa cystica back in 1891, as a
classical bone disease usually seen in severe
PHPTH. The popular term, “brown tumour” was given
by Jaffe owing to reddish brown colour of the
lesion due to the high vascularity and hemosiderin
pigment. Increased bone resorption on both
subperiosteal and endosteal surfaces due to high
circulating levels of PTH, led to the misnomer for
this entity, and “osteoclastoma” is often used.
These lesions are non-neoplastic, resulting from a
reparative process histologically [4]. In this
report, we have reviewed literature where BT was
the first presentation of PHPTH along with
comparison of age, sex and site of presentation
[Table 1].
| Table 1:
Reported Cases of Brown Tumor Associated
with PHPTH with Pathological Fractures as
the Primary Presentation |
| Year |
Study (First Author) |
No. of cases |
Sex |
Age |
Site |
| 2025 |
Our Case 1 |
2 |
M |
43 |
Neck femur |
| Our Case 2 |
M |
36 |
Humerus |
| 2023 |
Haouzi et al [7] |
1 |
F |
30 |
Subtrochanteric pathologic fracture of her
left femur |
| 2023 |
Aldosari et al [1] |
1 |
M |
21 |
Neck femur |
| 2022 |
Saini et al [2] |
1 |
F |
19 |
Distal Tibia, Fibula |
| 2021 |
Nguyen et al [8] |
1 |
F |
41 |
Peri trochanteric femur |
| 2020 |
Adegoke et al [5] |
1 |
F |
37 |
Pathological fractures of the right 9th
rib, anterior wedge compression, and
reduction of T4 vertebrae with other
abnormalities at T4–T5, T5– T6, T7–T8,
T10–T11, and L4–L5 vertebrae |
| 2020 |
Gosavi et al [4] |
1 |
F |
30 |
Mandible |
| 2015 |
Huang et al [6] |
3 |
M |
43 |
Mandible |
| M |
25 |
Both upper and lower extremity, multiple
sites |
| M |
42 |
Distal Tibia and 5th metatarsal |
| 2013 |
Olatoke et al [9] |
1 |
M |
21 |
Fracture of five long bones on four
separate occasions |
| 2008 |
Rachha Rajesh [10] |
3 |
F |
51 |
Right Femur |
| F |
32 |
Right Femur |
| F |
20 |
Left Humerus |
BT are seen commonly
in females and more common in people in their 4th
and 5th decade [5]. However, both our
cases and the cases reported by Aldosari et al and
Ruibin et al were seen in young and middle aged
male patients [1,6]. Frequently involved sites are
craniofacial bones then the long bones and ribs
[6]. In our cases, as well as study by Haouzi et
al and Saini et al., lesions were localised in the
long bones [2,7]. BT with their rare incidence
shows late manifestation in PHPTH. Contrary to
this in both our cases these lesions were caught
on early. BT has a higher incidence of 13% in
secondary HPTH. Main causes of PHPTH are
parathyroid adenoma, accounting for 85%,
parathyroid hyperplasia, accounting for 10–15%,
and carcinoma, accounting for 1–5% [4]. The
clinical presentation are variable ranging from
muscle weakness fatigue stones recurrently and
fractures [1]. PHPTH leads to high concentration
of calcium and phosphorus which causes urinary
stones caught on abdominal ultrasound or on a CT
scan easily and early [8]. Both our cases had a
history of repeated fractures
Radiologically BT
are often misdiagnosed for metastases or even
primary cancer when they present as diffuse
osteolytic lesions large lytic lesions [9].
However, histopathological evaluation is the gold
standard and IHC correlation is always preferred.
Microscopically BT represent localized
proliferation of fibrous tissue and giant cells,
which can replace bone and may produce osseous
expansion. Differential diagnoses can be many like
giant cell lesions such as solid aneurysmal bone
cyst (solid ABC), giant
cell tumor of bone (GCTB)
and giant cell reparative granuloma (GCRG) [6].
Solid ABC on histopathology shows large cystic
spaces and fibrous septa showing scattered
multinucleated giant cells along with rimming of
osteoblasts around the reactive woven bone. GCTB
has often been confused with BT, where the
osteoclastic giant cells are more evenly spaced,
the stromal cells are plumper and not so spindly
as in BT, and osteoblastic activity is less
conspicuous. The distinction with GCRG may be
impossible on morphologic grounds because both
lesions have a predilection for the jaw and their
microscopic appearances are essentially the same;
therefore the distinction is based on laboratory
findings and history [6]. Immunohistochemistry
(IHC) can also be of use here. Negativity for IHC
markers TRAP and cathepsin K in the multinucleated
giant cells of BT was studied and suggested by
Toriu et al in cases of diagnostic dilemmas [3].
Complete surgical resection in hyperfunctioning
parathyroid tissue is crucial for curative
treatment of PHPTH [9]. It is important to
identify BT from other benign bone lesions, at an
earlier stage in order to reduce the morbidity and
to prevent over diagnosis/ aggressive treatment of
metastasis/ primary bony malignancies.
Conclusion
These two cases
emphasise the need of inclusion of Brown Tumor in
the differential diagnosis of pathological
fractures or multifocal osteolytic bone lesions,
to not only avoid unnecessary surgical
interventions but for more extensive work up with
serum phosphate calcium and PTH levels, along with
imaging. As seen in both our cases, BT can be
masked by fractures at the time of presentation.
Thus, evaluation of debrided tissue of these
fracture sites cannot be emphasised enough as
histopathology is most definitive for the
diagnosis. The histopathological differentials of
solid aneurysmal
bone cyst, giant
cell tumor of bone and giant
cell reparative granuloma
though seemingly similar on morphology have
their distinct nuanced differences which need to
be evaluated thoroughly on microscopy.
References
- Aldosari S, Alghamdi EA, Alragea A. Multiple
Brown Tumors in Primary Hyperparathyroidism
Causing Pathological Fracture: A Case Report of
a 21-Year-Old Adult Male. Cureus. 2023
Mar 10;15(3):e35979.
- Saini V, Gupta N, Mohan A et al. Osteitis
Fibrosis Cystica: Classical Case Report of an
Uncommon Presentation in a Young Female. Indian
J Otolaryngol Head Neck Surg 2022;74
(Suppl 3):5319–5323.
- Toriu N, Ueno T, Mizuno H, et al. Brown tumor
diagnosed three years after parathyroidectomy in
a patient with nail-patella syndrome: A case
report. Bone Rep. 2018 Dec
10;10:100187.2018.
- Gosavi S, Kaur H, Gandhi P. Multifocal
osteolytic lesions of jaw as a road map to
diagnosis of brown tumor of hyperparathyroidism:
A rare case report with review of literature. J
Oral Maxillofac Pathol 2020;24:S59-66.
- Adegoke OO, Ajani MA, Awosusi BL, Onakpoma FA,
Saiki O, Daniel A. Parathyroid Adenoma with
Unusual Presentations of Rib Bone and Thoracic
Vertebrae Fractures in a Premenopausal Female in
Ibadan, Nigeria. Niger Med J.
2020;61(5):273-275.
- Huang R, Zhuang R, Liu Y, Li T, Huang J.
Unusual presentation of primary
hyperparathyroidism: report of three cases. BMC
Med Imaging. 2015;15:23.
- Haouzi MA, Benbouzid Y, Baidriss Y, Kharmaz M,
Zouaidia F, Sfar K. Pathological subtrochanteric
fracture revealing a primary
hyperparathyroidism: A case report. Int J
Surg Case Rep. 2023;106:108158.
- Nguyen GN, Nguyen LV. The pathology femoral
peritrochanteric fracture with multiple brown
tumor as a first sign of parathyroid cancer - A
case report. Int J Surg Case Rep. 2021;85:106259.
- Olatoke SA, Agodirin OS, Rahman GA, et al.
Serial pathologic fractures of five long bones
on four separate occasions in a patient with
primary hyperparathyroidism, challenges of
management in a developing country: a case
report. Pan Afr Med J. 2013;15:45.
- Rachha R. Pathological Fractures as the
Presenting Symptom of Parathyroid Adenoma: A
Report of Three Cases. British Journal of
Medical Practitioners. Sept.
2008;1(1):26-29.
|



















