|
Introduction
Thyroglossal
duct cysts (TGDC) develop from the residues of the
thyroglossal duct, which usually regress at 6th
to 8th week of gestational life [1,2].
One of the most common inborn anomaly, its
prevalence is reported to be approximately 7%
among the general population [3]. These cysts can
manifest as a fistula, duct, cyst or ectopic
thyroid tissue [3]. The residual thyroid tissue
may persist within the duct, and its
transformation can result in thyroglossal duct
carcinoma [2]. First described in 1911, this
condition has a slightly higher incidence in women
than men (2.1:1) and typically manifests in middle
age [2,3].
Malignancy occurring
in TGDC is extremely rare, with a reported
incidence of 0.7% to 1%. Papillary thyroid
carcinoma is the most common histological type
which is most often diagnosed postoperatively
through histopathological examination [3-5].
Despite being a rare occurrence, PTC in a TGDC has
several challenges with respect to preoperative
diagnosis and therapeutic strategies adopted.
Clinical symptoms in a TGDC and malignancy arising
in TGDC are usually nonspecific. Moreover, FNAC
has low accuracy in view of the cystic nature of
these lesion, accounting for a false negative
diagnosis[5,6]. The therapeutic modalities opted
for PTC arising in TGDCs are deduced from the
general management guidelines of thyroid PTC,
which may not be absolutely pertinent in view of
difference in lymphatic drainage, anatomy and
embryology [5]. Most of the PTC in TGDCs are
diagnosed post surgically. Whether completion
total thyroidectomy and or radioiodine therapy is
required in these cases is still a matter of
debate [7,8].
Rarity of the
disease and lack of consensus on management
guidelines, makes the case documentation critical
in order to add information to the existing
literature. Hence we report a case of PTC in TGDC
highlighting the pitfalls of the preoperative
diagnostic modalities, the importance of
harbouring high index of clinical suspicion and
the significance of careful pathological
examination of excised TGDCs to identify such
unexpected findings.
Clinical Presentation
A
60-year-old female patient presented to ENT
outpatient department with a persistent swelling
in the midline of her neck, which had been present
for the past eight to nine years. The swelling had
an insidious onset and gradually increased in size
over time. Despite the progression, the patient
did not experience any associated symptoms such as
pain, difficulty in swallowing solids or liquids,
or hoarseness of voice. The patient had been
otherwise healthy prior to the development of this
swelling, with no significant medical history or
prior surgeries or any family history. She did not
report any known allergies to food or medications.
Despite the
long-standing swelling, the patient reported a
history of consuming Tab.Thyronorm for only 20
days. On physical examination, a solitary swelling
approximately 5 x 5 cm in size was noted at the
anterior aspect of the neck, more prominent on the
left side. The swelling extended to the
sternocleidomastoid muscle bilaterally. The
inferior border of the swelling could not be
palpated. The swelling was observed to move with
deglutition but did not move with protrusion of
the tongue. The trachea appeared to be central.
The swelling had a smooth, regular surface and was
firm in consistency. The skin over the swelling
was pinchable, and the swelling was freely mobile
in both horizontal and vertical directions.
A thyroid
ultrasonography examination (USG) was performed,
which revealed a well-defined spongiform nodule in
the right lobe of the thyroid, classified as
TIRADS I, suggesting benign findings. The isthmus
showed a well-defined isoechoic area with
circumferential calcification, classified as
TIRADS III, likely benign. The left lobe presented
a well-defined anechoic cystic lesion, classified
as TIRADS 0.
FNAC was performed
under ultrasound guidance. FNAC smears from all
three lesions, as mentioned in the USG report,
showed similar morphology. Smears showed
follicular cells in small clusters along with cyst
macrophages, singly and in clusters, in a
background of thick and thin colloid. A diagnosis
of benign nodule possibly colloid goitre was made.
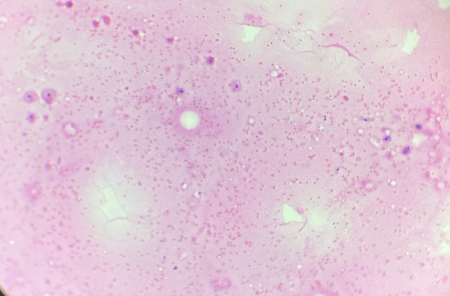
(Figure 1)
|
|
| Figure
1: Smears show only cyst macrophages and
think colloid (Haematoxylin and Eosin, x
100) |
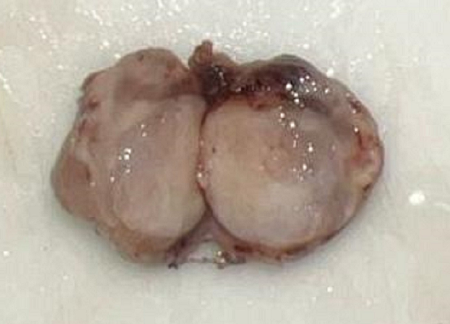
Figure
2: Firm nodule in the upper pole of
isthmus. Cut surface showed solid areas.
|
Further imaging with
a Contrast-Enhanced Computed Tomography (CECT) of
the neck revealed a large, well-defined mixed
solid-cystic lesion involving the isthmus and left
lobe of the thyroid, which was again reported as
likely of a benign etiology.
Given the above
findings, a left hemi thyroidectomy was performed.
On table the surgeon observed the thyroglossal
duct which could be traced down to a on the upper
margin of the isthmus. On palpation, surgeon
observed the nodule to be firm to hard. The firm
mass was excised. The excised specimen was sent
for histopathological examination (HPE).
On gross examination
the hemi thyroidectomy specimen measured 7.8 x 8.8
x 3.6 cm. The external surface was grey-brown with
attached capsule. On cut section, red-brown fluid
was expelled. On inspecting the cut surface few
grey-white fibrotic areas were noted. On
microscopy examination this lesion was reported as
Colloid Goitre with Hashimoto’s Thyroiditis.
Also received was
another specimen which consisted of a single,
irregular, grey-tan soft tissue bit measuring 2.8
x 1.9 x 1 cm. (Figure 2) On cut surface a lumen of
duct was identified and the tissue was firm in
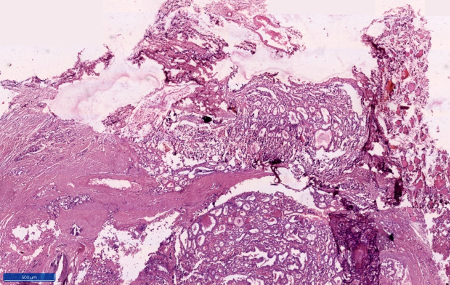
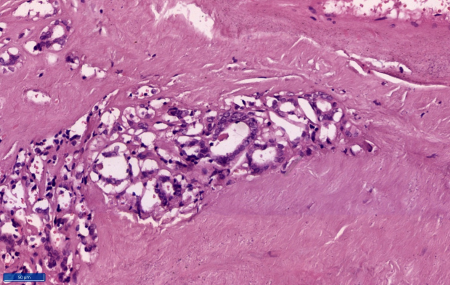
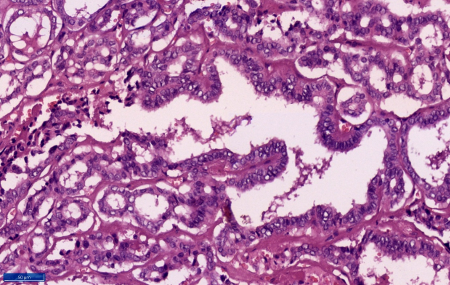
consistency. At microscopy sections showed a duct
made up of fibrous wall with extensive calcific
areas. The lumen of the duct showed a tumor
comprising of cells in predominantly papillary
pattern along with occasional follicle formations.
Individual cells lining the papillae and the
follicles showed crowding and overlapping. These
tumour cells demonstrated moderate eosinophilic
cytoplasm, mild nucleomegaly, round to oval with a
single nucleus showing nuclear clearing,
margination of the chromatin and occasional intra
nuclear grooves. Scanty mitosis were also noted.
The wall of the duct shows normal thyroid
follicles and chronic inflammation. The tumour
cells were embedded in the duct walls at places.
However, tumour cells were not extending beyond
the duct. (Figure 3-6) Hence a final diagnosis of
papillary carcinoma of thyroid-classic type (PTC),
arising in a thyroglossal duct cyst was made.
Patient is doing well one year post surgery.
Institutional ethical clearance was obtained from
the institutional ethical committee for
publication of the as report.
|
|
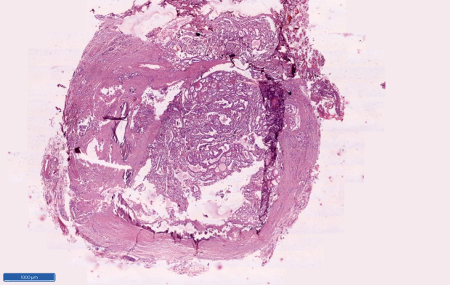
| Figure
3: Section shows cyst with tumour within
it (Haematoxylin and Eosin, x 40) |
Figure
4: Section shows protrusion of tumour
cells outside the capsule (Haematoxylin
and Eosin, x 100) |
|
|
| Figure
5: Section shows tumour cells trapped
within the cyst wall. (Haematoxylin and
Eosin, x 100) |
Figure
6: Section shows tumoral papillae line by
tumour cell showing nuclear crowding,
overlapping, nuclear clearing and
grooving. (Haematoxylin and Eosin, x 400) |
Discussion
The profound rarity
of thyroglossal duct cyst carcinoma (TGDCC) is
evidenced by reported incidences in literature
typically ranging from less than 1% to
approximately 1.5% of all TGDC cases, underscoring
the importance of early recognition, accurate
diagnosis and proper management; especially in the
era of personalised oncology care. Among all the
histologic types of malignancies, papillary
carcinoma is most common, seen in 80 to 94% cases.
Rarely squamous cell carcinoma, follicular and
anaplastic carcinomas have been reported to occur
in TGDC[4,6,9].
Diagnosis of TGDCC
is most frequently made postoperatively, primarily
through careful histopathological evaluation
following surgical removal of the cyst.
Preoperative evaluations like USG and FNAC
frequently suggest a benign lesion, as was
observed in the present study. However, the
operating surgeon, in the present study observed a
firm to hard mass at the end of the thyroglossal
duct which was excised[8,9].
The thyroid gland
descends from the base of tongue through the
thyroglossal duct to its final position in the
neck. There may be remnants of thyroid tissue
anywhere in its path which is regarded as ectopic
thyroid tissue which normally atrophies[1]. But,
persistence of it, potentially leads to the
formation of cysts. These remnants of ectopic
thyroid tissue within the cyst wall are considered
the primary site of origin for papillary thyroid
carcinoma in TGDCs[3,4]. The presence of thyroid
follicles in the cyst wall, as observed
histologically, further supports this theory. Few
authors have been suggesting that papillary
carcinoma in a TGDC could represent metastasis
from a primary thyroid tumour, but this phenomenon
is rare [1,2]. The frequent co-occurrence of
papillary carcinoma in both the TGDC and the
normally located thyroid gland is often
interpreted as synchronous primary tumours arising
independently in ectopic and orthotropic thyroid
tissue, rather than a metastatic event. In the
present case report, the thyroid gland did not
show any evidence of malignancy [2,4]. The exact
pathogenesis of PTC occurring in TGDC is unknown,
however the role of molecular alterations BRAF
V600E, RET/PTC gene rearrangements akin to that
seen in PTC of thyroid gland has been reported
[2].
While TGDC are more
commonly seen in younger individuals, TGDCC is
more likely to be diagnosed in adults, typically
in third and fourth decade of life, making the
patient's age a relevant factor when considering
the possible diagnoses. A midline painless neck
swelling is routinely a presenting feature for
TGDCCs, but it is not specific for malignancy.
While suspicious signs like fixation, firmness, or
rapid growth may indicate malignancy but are not
definitive. TGDCC are diagnosed late either as
intraoperative findings on frozen section or post
operatively on histopathological examination. In
the present case report, a 60-year-old woman came
with a long standing midline swelling in front of
neck, slow growing, firm in consistency, freely
mobile and was painless. This presentation is
nonspecific and does not provide any clue for a
PTC arising from a thyroglossal duct cyst. This is
similar to the existing literature which points
out that such carcinomas often have an indolent or
asymptomatic presentation and are mostly diagnosed
post-surgery due to their similarity to benign
thyroglossal duct cysts [1,2,5].
Radiological
modalities like USG and CECT play a key role in
the preliminary evaluation of TGDCs [2,4,5,7,11].
While these imaging techniques can highlight
characteristics that suggest a possible malignancy
within the cyst (TGDCC), they typically lack
definitive diagnostic value on their own [2,8].
While USG can identify features such as
calcification, lymphadenopathy, and solid
components within a cyst, CECT can give a clear
picture of the extent of the lesion and its
relationship with adjacent structures. In the
present case, the thyroid USG showed calcification
in the isthmus which was interpreted as TIRADS
III, and the CECT scan showed a large mixed
solid-cystic lesion involving the isthmus and left
lobe of the thyroid, which was likely benign. This
is concordant with the findings of Mahajan et al.,
Kirmani et al., and Bu et al. who suggested that
the presence of calcification within a
thyroglossal duct cyst should increase suspicion
for carcinoma [2,6,12]. Additionally, Kirmani et
al., Mahajan et al., and Srivanitchapoom et al.
pointed out that USG showing a central solid
component is a predictor of malignancy in
suspected TGDCs [6,12,13]. Despite the presence of
calcification and a mixed lesion in this case,
which can be associated with malignancy, the
initial radiological assessment favoured a benign
aetiology, underscoring the inherent limitations
of imaging in definitively diagnosing TGDCC.
Though FNAC is a
highly sensitive tool in triaging patients with
thyroid lesions, its role in TGDCC is often
limited by scanty cellularity and cystic nature of
the lesion [5,13]. Few of the TGDCCs find place in
the indeterminate category, especially when the
cells show degenerative atypia due to their
presence in cystic fluid further adding to the
diagnostic dilemma[5,7]. However, recent progress
in molecular cytology allows application of
mutational and gene expression analysis for risk
stratification of such indeterminate cases [1,2].
Following surgical
excision of a suspected thyroglossal duct cyst,
HPE is crucial for definitive diagnosis,
especially with long standing TGDCs.
Histopathology report confirmed the unexpected
finding of papillary carcinoma in the thyroglossal
duct cyst. However, the left lobe and isthmus of
thyroid gland revealed the presence of colloid
goitre with Hashimoto's thyroiditis.
HPE of PTC in TGDC
shows classical features of PTC like true
papillae, distinctive nuclear features consistent
with papillary carcinoma like nuclear enlargement,
nuclear grooves, and pseudo inclusions along with
psammoma bodies. However differentiating this from
a metastatic PTC is important in terms of
difference in prognostic and therapeutic
implications. Joseph and Komorowski et al proposed
following criteria for distinguishing PTC in TGDC
from metastatic PTC: i) presence of thyroglossal
duct remnant, ii) presence of ectopic thyroid
tissue in the cyst wall and iii) absence of PTC in
the thyroid gland. In the present case report all
three criteria were met [14].
Extent of the
surgery in TGDCCs is controversial. Similar to
TGDC, the standard surgical treatment for low risk
TGDCC is Sistrunk procedure. Here the cyst, the
central part of the hyoid bone, and a channel
extending towards the base of the tongue are
removed [4]. However in the presence of high risk
features like coexistent malignancy in thyroid
gland, lymph node metastasis, aggressive
histologic subtype, capsular invasion, total
thyroidectomy with radical neck dissection in
advocated[6,12]. Nevertheless, the decision to
over treat should not outweigh the risk of
surgical morbidity.
Radioiodine therapy
is indicated in TGDCCs cases who had undergone
total thyroidectomy. Regular follow-up usually
involves ultrasound examination and serum
thyroglobulin assay to monitor for any signs of
recurrence[1,8]. The prognosis of TGDCC is
excellent following total surgical excision[1,4].
Comprehensive review
of existing literature on TDCC is depicted in
table. [Table 1]
|
Table 1: Comprehensive review of
existing literature
|
|
Name of Author and year of publication
|
No of cases reported
|
FNAC findings
|
Radiology findings
|
Histologic type
|
Surgery performed
|
|
Salih, A. M, et al. 2024 [9]
|
10
|
"Suspicious for malignancy" (6/10),
"Negative for malignancy" (1/10), "Not
conducted" (3/10)
|
Cystic lesion (4/10), Complex lesion
(3/10), Cystic lesion with
microcalcification and mural nodule
(3/10).
|
Papillary Thyroid Carcinoma (PTC)
|
Sistrunk operation; Sistrunk + Total
thyroidectomy/lobectomy for concomitant
thyroid carcinoma
|
|
Mahajan A, et al. 2023 [12]
|
22
|
Pre-op FNAC mentioned as aiding
diagnosis/risk stratification. Not
detailed per case, but generally "atypical
cells" or "suspicious for PTC".
|
Irregular/lobulated margins (90.4%),
Solid-cystic composition (61.9%), Internal
vascularity (47.6%), Internal
calcification (76.19%) on US.
|
Papillary Carcinoma
|
Sistrunk procedure; selective nodal
dissection for suspicious nodes
|
|
Mettias B, et al. 2022 [11]
|
95 (patients operated for TGDC, not all
confirmed carcinoma in this specific
article, but focuses on overall TGDC
management)
|
Variable; 17% had FNAC, often showed
benign findings initially ("Insufficient
material" or "cystic contents" leading to
false negatives).
|
US (85% of patients had it), showed
normal thyroid in orthotopic position; 61%
infrahyoid. Not specifically detailed for
malignant features.
|
Papillary carcinoma (for the cases that
were malignant)
|
Sistrunk procedure (primary)
|
|
Srivanitchapoom C, et al. 2017 [13]
|
1
|
"Benign cystic lesion" with follicular
cells (false negative in this case).
|
Radiology reported TGDC; specific
malignant features not explicitly given.
|
Papillary Carcinoma
|
Sistrunk procedure; total thyroidectomy
considered
|
|
Kirmani OS, et al. 2016 [6]
|
7
|
Blind FNAC positive in 1 case; USG-guided
FNAC confirmed malignancy in 5/5 cases
where performed.
|
"Solid internal nodular component" with
"multiple tiny echogenic foci
(microcalcifications)" in all 7 cases;
enlarged lymph nodes in 3 cases.
|
Papillary Thyroid Carcinoma
|
Sistrunk procedure (implied)
|
|
Manipadam JM, et al. 2011 [7]
|
9
|
"Atypical cells" (2/5 cases where FNAC
was done); high rate of false
negatives/inadequate specimens due to
cystic nature.
|
Suspicious lesion in 4/6 cysts on
imaging; solid components and
calcification were 100% predictive of
carcinoma.
|
Papillary Thyroid Carcinoma
|
Sistrunk procedure (all cases); some also
had thyroidectomy
|
|
Kalyani R, et al. 2015. [3]
|
1
|
"Nodular goiter" or "cystic lesion" in
some instances; true positive in 66% of
cases.
|
Painless midline neck swelling; moved
with deglutition and tongue protrusion.
Imaging showed a cystic mass.
|
Papillary Carcinoma
|
Sistrunk's procedure (often followed by
total thyroidectomy)
|
|
Agarwal K, et al. 2010 [10]
|
1 (discusses 15 cases reported previously
with FNAC)
|
Positive for PTC in 9/15 cases previously
reported; false negative due to cystic
fluid/hypocellularity.
|
Neck exploration showed cystic mass; US
of neck revealed slightly hypoechoic
midline neck mass.
|
Papillary Carcinoma
|
Sistrunk's operation; total thyroidectomy
|
|
Miccoli P, et al. 2004 [15]
|
18
|
Not primary focus, often diagnosed
post-op on histopathology.
|
Not detailed in summary of this
particular series.
|
Papillary Carcinoma (16), Follicular (2)
|
Sistrunk procedure; Total thyroidectomy
|
|
Heshmati HM, et al. 1997 [16]
|
12
|
Diagnosis made after Sistrunk procedure
in 11/12 cases; preoperatively in 1 case
by FNA.
|
Midline upper neck mass; further imaging
details not explicitly given in the
abstract.
|
Papillary Carcinoma (all)
|
Sistrunk procedure; 9 patients had
subtotal/near-total thyroidectomy
|
Conclusion
This
case report highlights the importance of
considering malignancy, however infrequent, in the
differential diagnosis of TGDC masses, even in the
absence of overt suspicious features. The case
underscores the need for thorough pathological
examination of excised TGDCs to identify such
unexpected findings. Recent advances in
radiological, molecular and cytological approaches
can pave way for accurate preoperative diagnosis,
ensuring personalized therapeutics. Further
literature on individual case reports, or series
or multi-institutional studies are required which
could serve as data base for formulation
management guidelines for this uncommon
malignancy.
References
- Colino M, Breda D, Sepodes B, Melo C, Barroso
LA. Early diagnosis of papillary carcinoma in a
thyroglossal duct cyst: A multidisciplinary
approach and the crucial role of fine-needle
aspiration cytology. Cureus. 2024;16:e71254.
- Bu F, Yu K, Dong B et al. Research progress of
ectopic thyroid cancer in thyroglossal duct
cyst: A case report and literature review. Medicine.
2024;103:e38540.
- Kalyani R, Hebbar A, Murthy VS. Primary
papillary carcinoma arising in thyroglossal duct
cyst: a rare case report. Natl J Lab Med.
2015;4:27-29.
- Sánchez G, Ariza A, Sánchez S et al. Papillary
thyroid carcinoma in thyroglossal duct cysts:
case series with long-term follow-up and review
of the literature. Ann Mediterr Surg.
2023;6:04-10.
- Mittal A, Sandhu A, Chhetri M, Jaiswal G. A
rare case of thyroglossal duct cyst cancer and
literature review. J Clin Transl Endocrinol
Case Rep. 2023;1:36.
- Kirmani OS, Bashir S, Firdose SR et al.
Ultrasonography of thyroglossal duct cyst;
central solid component as a predictor of
malignancy– experience with seven cases. Sch
Acad J Biosci. 2016;4:312-7.
- Manipadam JM, Manipadam MT, Thomas EM et al.
Thyroglossal duct carcinoma: a case series and
approach to management. World J Endocr Surg.
2011;3:59-63.
- Yankov YG, Stoev L, Dimanov S, Stoeva M,
Stanislavova K. A rare case of papillary thyroid
carcinoma in the thyroglossal duct cyst of a
14-year-old female patient with left thyroid
hemiagenesis. Cureus.
2023;30:e49712.
- Salih AM, Qaradakhy AJ, Saeed YA et al.
Carcinoma arising from thyroglossal duct
remnants. Biomed Rep. 2024;20:60.
- Agarwal K, Puri V, Singh S. Critical appraisal
of FNAC in the diagnosis of primary papillary
carcinoma arising in thyroglossal cyst: A case
report with review of the literature on FNAC and
its diagnostic pitfalls. J Cytol.
2010;27:22-6.
- Mettias B, Cole S, Valsamakis T. Preoperative
investigations in thyroglossal duct cyst
surgery: a 9-year experience and proposed
practice guide. Ann R Coll Surg Engl. 2023;105:554-60.
- Mahajan A, Deokar S, Suryavanshi S et al. Role
of imaging in the management of thyroglossal
duct cyst carcinomas (TGC-TIRADS): a single
centre retrospective study over 16 years. Front
Oncol. 2023 Sep 21;13:1201774.
- Srivanitchapoom C, Sittitrai P, Yata K,
Khongpiboonkit P. Ultrasonographic findings of
thyroglossal duct papillary carcinoma: A case
report. Int J Surg Case Rep.
2017;32:54-7.
- Joseph TJ, Komorowski RA. Thyroglossal duct
carcinoma. Human Pathology. 1975;6:717–729.
- Miccoli P, Minuto MN, Galleri D, Puccini M,
Berti P. Extent of surgery in thyroglossal duct
carcinoma: reflections on a series of eighteen
cases. Thyroid. 2004 Feb;14:121-3.
- Heshmati HM, Fatourechi V, Van Heerden JA, Hay
ID, Goellner JR. Thyroglossal duct carcinoma:
Report of 12 cases. Mayo Clinic Proceedings.
1997;72:315-319.
|



















