|
Introduction
Normal
oral mucosa is a soft tissue membrane that
stretches posteriorly from the palatopharyngeal
folds to vermilion edge of the lips anteriorly.
Dentists are typically the first to notice any
variation in the oral cavity's natural features. A
wide range of factors, including infections
(bacteria, fungus, viruses, parasites, and
others), physical and environmental factors,
immune system changes, systemic disorders,
neoplasia, trauma, and others, can induce changes
in the oral mucosa [1].
Oral lesions
commonly encountered in the dental practice either
reflect disease or trauma which could result from
any physical, chemical or thermal insults. Trauma
associated with road traffic accidents is
primarily seen on hard tissues like jaw fractures
while trauma associated with soft tissue lesions
is encountered in routine daily activities while
brushing and chewing. Another side of this
spectrum lies the self-inflicted injuries like
lip/ cheek biting, thermal or chemical burns and
even from iatrogenic causes like defective
dentures, orthodontic brackets or other treatments
involving oral cavity such as intubation under
general anesthesia [2]. So, trauma can have
multifaceted presentation in oral cavity ranging
from a minor oral ulcer to a malignant lesion and
no age group and gender is exempted from these
traumatic lesions. They can hamper basic processes
like feeding, swallowing, speech and are also
typically accompanied with pain and suffering.
Oral traumatic lesions differ from other oral
lesions in clinical presentation and progression.
Some of them could be acute lesions while majority
are chronic in nature. A thorough history and
clinical examination is mandatory to trace the
traumatic cause of such pathologies. Although
trauma associated injuries are usually not
subjected to histopathological examination, but
soft tissue trauma should be kept as differential
diagnosis while dealing with the soft tissue
pathologies.
Extensive search on
scientific data in English literature, revealed
relatively rare studies on trauma-associated
lesions in oral and maxillofacial region in
developing Asian countries and those that do exist
are typically restricted to studies of fractures
of the jawbone or traumatic injuries to teeth with
no emphasis on soft tissue trauma [3]. This has
resulted in neglect of a wide category of
traumatic pathologies occurring in oral mucosa
leading to diverse array of histopathological
diagnosis.
In order to better
understand the demographics of such soft tissue
traumatic lesions a histopathological study was
planned that included data spanning over past 12
years. The study findings made us realize that
traumatic oral pathologies are actually a huge
spectrum that include diverse histopathological
diagnosis and sometimes early intervention is
anticipated.
Materials and Methods
A retrospective cross-sectional study was
conducted in Department of Oral and Maxillofacial
Pathology, PGIDS, Rohtak, Haryana by retrieving
demographic data and recording chief complaints
from the requisition forms mentioning anywhere in
the form the term “trauma” of any nature,
“accident”, “history of fight” or any other type
of “physical abuse”. This data was obtained from
January 2010- December 2022. Ethical approval was
taken from institutional ethical committee vide
letter no. PGIDS/BHRC/24/29.
Study sample
All patient biopsy
requisition records in the department for the
specified time period were analyzed and all cases
with a mentioned history of trauma were included
in the study and those without were excluded from
study. Of the 5,468 patient’s data analyzed, 307
cases favoring the inclusion criteria were
selected for final evaluation.
Sample type
The biopsy
requisition record of patient with documentation
on previous medical and dental history were noted.
The data collected included demographic data
mentioned in medical records, data on trauma
history, type of injury, duration and site of
injury and the histopathological diagnosis was
confirmed by two experienced oral and
maxillofacial pathologists. The data was then
entered in Microsoft excel and analyzed.
Results
From the total 307
cases analyzed, the male (201) to female (106)
ratio was 1.8:1. The patients’ age ranged from
five to eighty years with the mean age being
33.24. The traumatic oral lesions and demographic
data are presented in Table 1. The oral lesions
associated with trauma included soft tissue
lesions like mucocele, traumatic fibroma,
fibroepithelial hyperplasia (FEH) and periapical
lesions. The youngest patient was diagnosed with
traumatic fibroma while oldest had
well-differentiated oral squamous cell carcinoma
(WD-OSCC).
Mucocele was the
most common oral lesion with history of trauma
(40.7%) followed by traumatic fibroma (27.6%) and
fibroepithelial hyperplasia (FEH) (11.4%). The
presenting complaint of patients varied from
swelling, growth, pain, ulcer and restricted mouth
opening from which the most common presentation
was swelling (71.8%). Considering the site of
lesion, the lower lip was the most commonly
involved site (42.7%) followed by buccal mucosa
(29.7%). The time duration between the time of
trauma and symptom of the lesion was found
different with different cases. The time period
between trauma to initial presentation of lesion
was found with a range of 14 days to >6 months
(Table 1).
|
Table 1: List of observed
traumatic oral lesions revealing site of
distribution, duration and clinical
presentation
|
|
Lesion
|
No of cases
|
Most common site
|
Duration for presentation from
initial trauma
|
Most common clinical presentation
|
|
Mucocele
|
125 (40.7%)
|
Lower lip
|
14 days – 3 months
|
Swelling
|
|
Traumatic fibroma
|
85 (27.6%)
|
Buccal mucosa
|
> 6 months
|
Swelling
|
|
Fibroepithelial hyperplasia
|
35 (11.4%)
|
Buccal mucosa
|
> 6 months
|
Swelling
|
|
Periapical cyst
|
17 (5.5%)
|
Anterior maxilla
|
> 6 months
|
Swelling
|
|
Periapical granuloma
|
12 (3.9%)
|
Anterior maxilla
|
14 days – 1month
|
Swelling and pain
|
|
Squamous cell carcinoma
|
22 (7.1%)
|
Buccal mucosa
|
1-3 months
|
Pain and ulcer
|
|
Lymphoepithelial cyst
|
2 (0.6%)
|
Buccal mucosa
|
> 6 months
|
Swelling
|
|
Pyogenic granuloma
|
2 (0.6%)
|
Buccal mucosa
|
14 days – 1 month
|
Swelling
|
|
Hemangioma
|
4 (1.3%)
|
Tongue
|
14 days – 1 month
|
Swelling
|
|
Verrucous carcinoma
|
3 (0.9%)
|
Buccal mucosa
|
1-3 months
|
Swelling
|
Discussion
Oral cavity is
susceptible to many forms of physical, chemical
and thermal insults which can result in traumatic
injuries to jaw bones as well as soft tissue of
oral mucosa. The trauma associated with jaw
fractures does not warrant any biopsy and usually
heals uneventfully. However traumatic lesions in
oral mucosa may require attention and further
histopathological investigations. These lesions
appear as acute or chronic ulcers, mucositis,
reactive hyperplasia, or even as white or red
lesions which mimic other potentially malignant
disorders raising a concern for prompt diagnosis.
To the best of our
knowledge, this is the first study in this region
which attempted to find the prevalence of trauma
associated oral pathologies and proposed a working
classification for such entities based on the
frequency of its occurrence with trauma.
In the present study
a male preponderance with 65.4% was observed which
was similar to previous studies on oral lesions
which may indicate a higher incidence of trauma in
males who are involved more in physical activities
and parafunctional habits [3-5].Out of the lesions
analyzed, the most commonly encountered were
mucocele, traumatic fibroma and fibroepithelial
hyperplasia which contributed to 79.8% (245) of
the total traumatic oral lesions. Similar higher
incidence for mucocele as a traumatic lesion is
reported frequently in literature. [6, 7]. For
mucoceles, some studies have reported female
gender prevalence [8,11] while some [9,10] showed
a male gender predominance similar to that seen in
our study. Lower lip was the most common affected
site in our study as well as in literature
[6,7,8,9] (Figure 1 A and B). Given that the lower
lip moves dynamically during mastication and
speech, this can be primarily explained by the
fact that it is one of the oral locations most
susceptible to trauma during parafunctional or
functional activities. Patients with mucocele were
more common in age group of 19-44 years, with mean
age of 33.3 years and were generally younger than
those exhibiting traumatic fibroma which was found
more in age group of 45-64 years. The main
etiological reason for the mucus extravasation
phenomena is thought to be mechanical trauma,
mostly due to parafunctional habits, which is
thought to be more likely to occur in younger age
group [6,7].

|
| Fig 1: A.
Clinical presentation of mucocele on lower
lip B. Histologic presentation of mucocele
(4x) C. Clinical picture of
fibroepithelial hyperplasia on buccal
mucosa D. Histologic presentation of
fibroepithelial hyperplasia (10x). |
Traumatic fibroma
(85, 27.6%) and fibroepithelial hyperplasia (35,
11.4%) were the second and third most common
lesions encountered. A similar prevalence for
these reactive lesions has been reported [12, 13],
however authors also report a much higher
prevalence i.e., 48% [14]. This can be due to
geographical and lifestyle differences and the
fact that many such lesions are clinically
diagnosed but not biopsied. The most common
location observed was buccal mucosa in our study
whereas previous studies indicated towards a
predilection for gingiva for these lesions [12,
13] (Figure 1 C and D). The
increased incidence in younger age group and
involvement of buccal mucosa can be attributed to
increased parafunctional habits and irritation of
mucosa from orthodontic devices in these age
groups.
Periapical lesions
secondary to trauma which included periapical
cysts and granulomas together accounted for 9.4%
of total cases in present study. This increased
prevalence was seen in 0-18 age group, most
commonly associated with non – carious, non-vital
anterior teeth and presented mostly as a swelling
and was associated with pus discharge. The
increased prevalence associated with this age
group can be associated with increased incidence
of trauma due to fall in patients visiting our
institute.
Development of
malignancies due to trauma is rare but not
uncommon as continuous irritation from a sharp
tooth or prosthesis can lead to transformation of
a traumatic ulcer to oral squamous cell carcinoma.
In our study, a considerable number of traumatic
lesions (22, 7.1%) were found to be OSCC,
especially in older age group, with buccal mucosa
and tongue being most commonly involved. All the
patients reported the history of a faulty denture
use or a sharp tooth. Other lesions found in this
study included pyogenic granuloma and hemangioma
which although accounted less in number but are
usually associated with a traumatic history.
Maximum number of
soft tissue traumatic lesions in the present study
were in the age range of 19-44 years (156),
followed by 0-18 years (67) 45-64 years (64) and
least in 65-84 years (21). This was in contrast to
findings by other studies [4,5] which reported an
older age group prevalence. The difference can be
attributed to the fact that these studies included
all oral mucosal lesions, which may be habit
associated also, and habit prevalence increased
with age. On the other hand, our study focused
mainly on trauma associated lesions which were
reported more in younger age groups due to
increased awareness even for acute lesions in this
group. Another observation recorded was that a
traumatic ulcer of longer duration of more than 3
months could make the lesion suspicious for
malignancy as in our study traumatic ulcers showed
malignant transformation within time period of 3
months. However, few oral traumatic lesions like
mucocele, fibroma, periapical and pyogenic
granuloma showed small duration of presentation of
14 days from the time of trauma reflecting
reactionary response.
It was also observed
that 24.3% of these lesions recurred with
traumatic fibroma, mucocele and ulcers as the most
common recurring pathologies. These findings point
towards the significance of identification of the
etiology in traumatic pathologies as removal of
causes like sharp tooth and faulty denture
prevents the recurrence of these lesions.
Literature lacks a
proper classification for trauma associated oral
soft tissue pathologies and this study motivated
us to propose a working classification of this
common and widespread but frequently neglected.
Hence, we are proposing a classification system
based on the relationship between frequency of
occurrence of a lesion and traumatic etiology seen
in our institutional experience. We included the
findings of our study as well as those from the
literature in this classification (Figure 2).
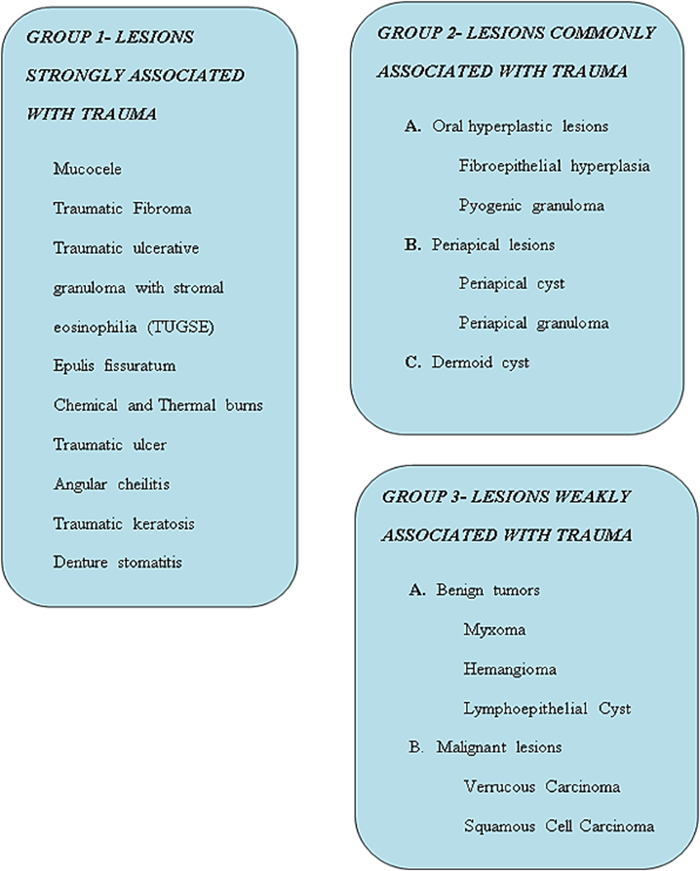 |
| Fig 2:
Proposed working classification of
traumatic oral pathologies |
Conclusion
Data from this study
will be helpful for epidemiological documentation
of the type of traumatic oral lesions as well as
educating about the significance of this group of
oral cavity lesions. Also, the proposed
classification will help in easy categorization of
traumatic oral pathologies. Knowledge about the
demographics of traumatic oral lesions can help us
in providing an insight into such common but
frequently neglected pathologies and sensitize the
practitioner for the cautionary follow up. Similar
attempts to identify and classify oral soft tissue
traumatic lesions from multiple centers will help
us to put weightage to our pioneer attempt.
References:
- Reichart PA. Oral mucosal lesions in a
representative cross-sectional study of aging
Germans. Community Dent Oral Epidemiol. 2000
Oct;28(5):390-8. doi:
10.1034/j.1600-0528.2000.028005390.x.
- Anura A. Traumatic oral mucosal lesions: a
mini review and clinical update. Oral Health
Dent Manag. 2014 Jun;13(2):254-9.
- Chen JY, Wang WC, Chen YK, Lin LM. A
retrospective study of trauma-associated oral
and maxillofacial lesions in a population from
southern Taiwan. J Appl Oral Sci. 2010
Jan-Feb;18(1):5-9. doi:
10.1590/s1678-77572010000100003.
- Patil S, Doni B, Maheshwari S. Prevalence and
distribution of oral mucosal lesions in a
geriatric Indian population. Can Geriatr J.
2015 Mar 31;18(1):11-4. doi:
10.5770/cgj.18.123.
- El Toum S, Cassia A, Bouchi N, Kassab I.
Prevalence and Distribution of Oral Mucosal
Lesions by Sex and Age Categories: A
Retrospective Study of Patients Attending
Lebanese School of Dentistry. Int J Dent. 2018
May 17;2018:4030134. doi: 10.1155/2018/4030134.
- Hong CHL, Dean DR, Hull K, Hu SJ, Sim YF,
Nadeau C, Gonçalves S, Lodi G, Hodgson TA. World
Workshop on Oral Medicine VII: Relative
frequency of oral mucosal lesions in children, a
scoping review. Oral Dis. 2019 Jun;25
Suppl 1:193-203. doi: 10.1111/odi.13112.
- Siadati S, Seyedmajidi M, Sharbatdaran M.
Frequency of different oral lesions in children
and adolescents in Babol, Northern Iran. Caspian
J Intern Med. 2013 Fall;4(4):773-6.
- Miranda GGB, Chaves-Junior SC, Lopes MP et al.
Oral mucoceles: A Brazillian Multicenter Study
of 1,901 Cases. Braz Dent J. 2022
Sep-Oct;33(5):81-90. doi:
10.1590/0103-6440202204965.
- Choi YJ, Byun JS, Choi JK, Jung JK.
Identification of predictive variables for the
recurrence of oral mucocele. Med Oral Patol
Oral Cir Bucal. 2019 Mar
1;24(2):e231-e235. doi: 10.4317/medoral.22690.
- Conceição JG, Gurgel CA, Ramos EA et al. Oral
mucoceles: a clinical, histopathological and
immunohistochemical study. Acta Histochem. 2014
Jan;116(1):40-7. doi:
10.1016/j.acthis.2013.04.015.
- Hayashida AM, Zerbinatti DC, Balducci I,
Cabral LA, Almeida JD. Mucus extravasation and
retention phenomena: a 24-year study. BMC
Oral Health. 2010 Jun 7;10:15. doi:
10.1186/1472-6831-10-15.
- Soyele OO, Ladeji AM, Adebiyi KE, Adesina OM,
Aborisade AO, Olatunji AS, Adeola HA. Pattern of
distribution of reactive localised hyperplasia
of the oral cavity in patients at a tertiary
health institution in Nigeria. Afr Health
Sci. 2019 Mar;19(1):1687-1694. doi:
10.4314/ahs.v19i1.45.
- Buchner A, Shnaiderman-Shapiro A, Vered M.
Relative frequency of localized reactive
hyperplastic lesions of the gingiva: a
retrospective study of 1675 cases from Israel. J
Oral Pathol Med. 2010 Sep;39(8):631-8.
doi: 10.1111/j.1600-0714.2010.00895.x.
- Ala Aghbali A, Vosough Hosseini S, Harasi B,
Janani M, Mahmoudi SM. Reactive hyperplasia of
the oral cavity: a survey of 197 cases in
tabriz, northwest iran. J Dent Res Dent Clin
Dent Prospects. 2010 Summer;4(3):87-9.
doi: 10.5681/joddd.2010.022.
|



















