|
Case
Report
Pancreatic
Ganglioneuroma in the Elderly: A Rare
Case in a 65-Year-Old Woman
Authors:
Swathi Prabhu,
Assistant Professor, Department of
Pathology,
Hansika N, Postgraduate
Student, Department of Pathology,
Sneha Khandelwal, Undergraduate
Student,
Anushka Acharya, Undergraduate
Student,
Nischitha Suvarna, Senior
Resident, Department of Pathology,
Vidya Monappa, Additional
Professor, Department of Pathology,
Naveena AN Kumar, Professor and
Head, Department of Surgical Oncology,
Kasturba Medical College - Manipal,
Manipal Academy of Higher Education,
Manipal, India.
Address for
Correspondence
Dr. Nischitha
Suvarna,
Senior Resident,
Department of Pathology,
Kasturba Medical College, Manipal,
Manipal Academy of Higher Education,
Manipal India.
E-mail:
nischitha.ns@manipal.edu.
Citation
Prabhu S, Hansika N,
Khandelwal S, Acharya A, Suvarna N,
Monappa V, Kumar NAN. Pancreatic
Ganglioneuroma in the Elderly: A Rare
Case in a 65-Year-Old Woman. Online
J Health Allied Scs.
2025;24(1):9. Available at URL:
https://www.ojhas.org/issue93/2025-1-9.html
Submitted:
Jan
12 , 2024; Accepted: Feb 25, 2025;
Published: Apr 15, 2025
|
|
|
|
|
Introduction
Ganglioneuroma
is a benign tumor derived from neural crest cells,
typically found along the sympathetic nervous
system, with common locations including the
mediastinum, adrenal gland, and the
retroperitoneum. Retroperitoneal and mediastinal
ganglioneuromas are typically seen in the
pediatric population, while adrenal
ganglioneuromas tend to occur in slightly older
individuals, around 35-40 years of age.[1]
Pancreatic localization of ganglioneuromas is
rare, with only a few case reports documented in
the literature.[2] They pose a significant
diagnostic challenge due to the complexity of the
procedure, lack of specific radiological features,
and typically poor cellular yield on fine needle
aspiration cytology (FNAC), owing to the fibrous
nature of the lesion. We present a case of
pancreatic ganglioneuroma, initially detected on
radiological imaging as a solid-cystic lesion with
differentials of lymphangioma or mucinous
cystadenoma. However, following surgical resection
and histopathological examination, the final
diagnosis was confirmed as ganglioneuroma.
Case history
A 65-year-old woman
presented with a one-year history of abdominal
discomfort. On physical examination, her vital
signs were normal, and the abdomen was soft and
non-distended, with no tenderness. Laboratory
tests revealed Carcinoembryonic antigen (CEA), CA
19-9, liver function tests were within normal
limits. Raised CA 19-9 levels in the cyst fluid
was observed.
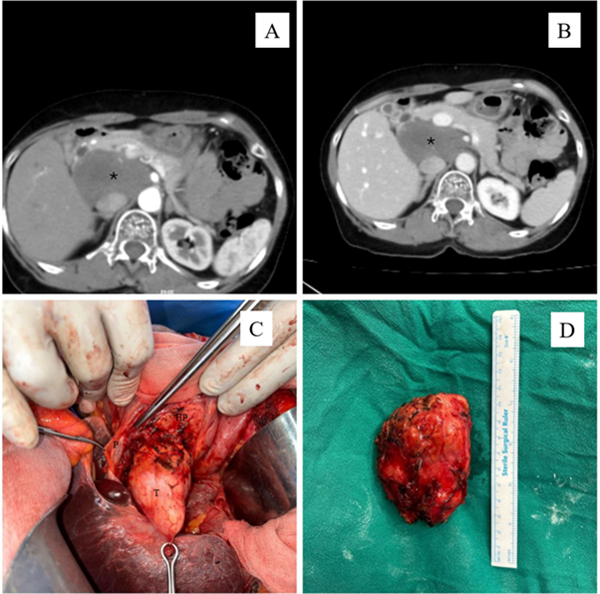
Abdominal and pelvic
CT with intravenous and oral contrast revealed a
large well-defined hypodense lesion, showing no
significant post contrast enhancement, noted in
the retroperitoneal region on the right, measuring
2.6 x 6.3 x 5.4 cm, corresponding to L1/L2
vertebral level with the head of the pancreas was
noted to be wrapping around the lesion. (Figure 1
A and B). Endosonography showed a large hypoechoic
lesion in retroperitoneum predominantly solid with
few cystic components. The preoperative diagnosis
in our case was cystic neoplasm of the pancreas.
FNAC was performed, revealing strips of epithelial
cells with mucin and goblet cells. Based on these
findings and the cystic appearance noted on
endosonography, the lesion was diagnosed as a
possible mucinous cystic neoplasm and
histopathology was requested for accurate
diagnosis. The surgical plan was enucleation vs
Whipple’s procedure. Intraoperatively, there was
well defined tumor adherent to posterior part of
head of pancreas and free from ampulla, pancreatic
duct and all vasculatures. As there was maintained
plane between the tumor and pancreas, it was
decided to go ahead with enucleation and avoiding
morbid Whipple’s procedure (Figure 1C and 1D).
|
| Figure
1: A large well-defined hypodense lesion
(avg. ~37 HU) located posterior aspect of
Head of Pancreas, showing no significant
post contrast enhancement measuring
2.6x6.3x5.4 cm A. arterial view. B. portal
view. C. Intraoperatively tumour was
adherent to posterior aspect of head of
the pancreas D- specimen with intact
capsule |
Postoperatively,
patient developed pancreatic fistula, which was
managed conservatively by keeping drain for 3
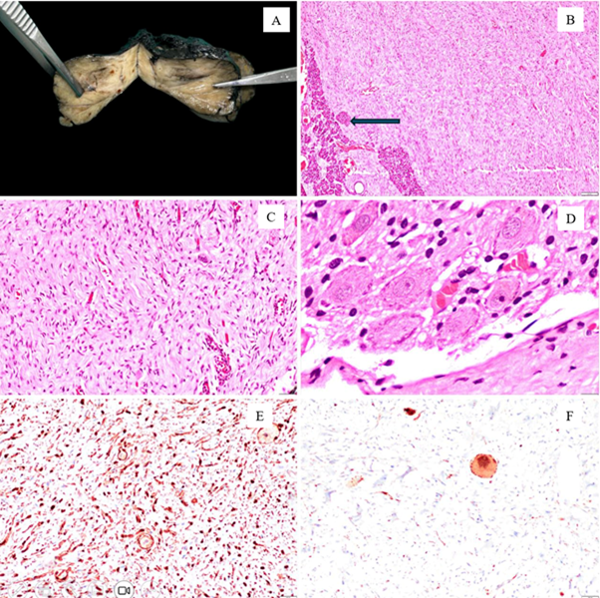
weeks. Gross examination of the specimen revealed
a predominantly solid mass with a few cystic
areas, measuring 6x5x2.5 cm and covered by serosa.
Adjacent normal pancreatic tissue was identified.
The lesion was well-circumscribed, firm,
glistening and white to yellow in colour (Figure
2A). Necrosis was not observed. Histopathological
examination revealed a final diagnosis of
ganglioneuroma (Figure 2B, C and D).
Immunohistochemical staining demonstrated S100
positivity highlighting the Schwannian stroma,
while synaptophysin marked ganglion cells (Figure
2E and F). The patient was discharged and is
currently under follow-up, four months after
discharge, with no complaints.
|
| Figure
2: Gross specimen of ganglioneuroma
showing predominantly solid lesion,
yellowish with fibrous to myxoid areas
(A), with pancreatic tissue (B). The
lesion shows Schwann cells arranged as
sheets admixed with ganglion cells (C).
Image D shows ganglion cells. S100
highlights the Schwannian stroma with
Schwann cells (E) with synaptophysin
positivity in the ganglion cells |
Discussion
Ganglioneuromas are
composed of a mixture of Schwann cells and
ganglion cells and are associated with the best
prognosis among peripheral neuroblastic tumors.
They are most commonly found in the thorax,
followed by the adrenal gland.[1] Including our
case, ten reported cases of pancreatic
ganglioneuromas have been exclusively observed in
females across all age groups. Ganglioneuromas are
rare, benign tumors that can occur across a wide
age range, from 3 to 86 years, with the majority
of cases reported in individuals under 30 years of
age. [2] Shaheen et al. documented a case in an
86-year-old patient, marking the upper limit of
this age spectrum. In our case, we report a
65-year-old woman, emphasizing that these lesions,
although rare, can also occur in older
individuals. Notably, this is only the second case
reported in the literature in a patient over the
age of 60.[3]
The pancreatic
origin of ganglioneuroma may arise from
peripancreatic nerves, with subsequent
infiltration into the pancreas, rather than
originating from within the pancreas itself. [2,4]
These tumors are typically asymptomatic, often
detected incidentally, or present with mild,
non-specific symptoms such as abdominal pain, back
pain, or vomiting due to compression of
surrounding structures.[1]
The radiological
findings of pancreatic ganglioneuroma are
non-specific, with CT typically showing a
low-attenuation mass and poor enhancement on
contrast-enhanced CT. [2,5] It is important to
note that the lesion may mimic as a cyst
radiologically, which could result in misdiagnosis
as a cystic neoplasm of the pancreas, as in our
case. [6] A core needle biopsy can be helpful for
preoperative diagnosis, as it allows usage of
immunohistochemistry (IHC) to aid in confirming
the diagnosis. Ultrasound-guided FNAC is often
less effective because of the fibrous nature of
the lesion and its low cellularity, which can lead
to a non-diagnostic aspirate or potential
misdiagnosis. However, accurate diagnosis can only
be made after resection. [7]
On gross
examination, lesions typically appear as solid,
well-circumscribed masses. Histopathological
examination shows a predominance of Schwann cells
admixed with ganglion cells which are dispersed
singly or clustered. Lymphoid aggregates can be
seen, which must be differentiated by neuroblasts,
using either IHC CD45 or synaptophysin.[1]
Surgical excision of
the lesion with adequate margins remains the
cornerstone of treatment.[2] Despite the proximity
to vital structures, the lesion generally has an
excellent prognosis, even if complete removal is
not achieved. Hence, authors recommend enucleation
unless the tumor infiltrating pancreatic
parenchyma. The Table 1 below summarises the
pancreatic ganglioneuroma cases reported in the
literature. [2-10]
|
Table 1: Demographic details, lesion
size, location, preoperative diagnosis,
treatment, and follow-up data of patients
diagnosed with ganglioneuroma
|
|
Authors
|
Age/sex
|
Size (mm)
|
Location
|
Preoperative diagnosis (cytology/biopsy)
|
Procedure
|
Follow up
|
|
Christein JD et al.[6]
|
28/F
|
65
|
Neck of the pancreas
|
frozen section: Negative for malignancy
|
Central pancreatectomy
|
Four years. No recurrence
|
|
Domanski HA. [8]
|
17/F
|
120
|
Head of the pancreas
|
FNAC*: Suspicious of ganglioneuroma
|
Enucleation
|
NR†
|
|
Poves I et al.[4]
|
33/F
|
40
|
Uncinate process of the pancreas
|
FNAC: Poor cellularity due to hard
consistency of the lesion. Negative for
malignancy
|
Resection of the uncinate process
|
NR
|
|
Ikoma N et al.[5]
|
4/F
|
33
|
Head of the pancreas
|
NR
|
pancreaticoduodenectomy
|
Three years. No recurrence
|
|
Scandavini C et al.[9]
|
3/F
|
NR
|
Head of the pancreas
|
NR
|
pancreaticoduodenectomy
|
239 months. No recurrence
|
|
Mazzola et al.[2]
|
30/F
|
70
|
Pancreatic tail
|
EUS-FNAB‡ : Suggestive soft tissue tumour
|
Distal pancreatectomy
|
Two years. No recurrence
|
|
Shaheen et al.[3]
|
86/F
|
13
|
Body of the pancreas
|
EUS-FNAB: Suggestive of ganglioneuroma
|
Not resected due to poor status of
patient due to advanced multiple myeloma
|
Four months later expired four months
from severe metastatic disease due to
multiple myeloma
|
|
Yildrim et al[7]
|
24/F
|
35
|
Neck of the pancreas
|
FNA: Spindle cell neoplasm
|
Resection of the neck of pancreas
|
Six months. No recurrence
|
|
Sanchez et al[10]
|
17/F
|
95
|
Head of the pancreas
|
US-guided percutaneous biopsy:
Ganglioneuroma
|
R2 resection due to encasement of the
celiac trunk
|
No recurrence (exact period not
mentioned)
|
|
Our case
|
65/F
|
63
|
Head of the pancreas
|
EUS-FNAC: Suggestive of mucinous
neoplasm. Histopathology confirmation was
advised
|
Resection with adequate margins
|
Four months. No recurrence
|
|
*FNA: Fine needle aspiration cytology
†NR: Not reported ‡ EUS-FNAB: Endoscopic
ultrasound fine needle aspiration biopsy
|
In conclusion,
pancreatic ganglioneuromas are extremely rare and
pose significant diagnostic challenges owing to
their non-specific clinical presentation,
radiological findings, and low cellular yield on
FNAC. Although, cytology can be helpful, accurate
diagnosis typically requires surgical excision and
thorough histopathological examination. Awareness
of this rare entity is crucial to avoid
misdiagnosis, particularly with cystic neoplasms,
and to ensure appropriate management and patient
care.
References
- Alaggio R, Hill DA, Jacques TS et al. WHO
Classification of Tumors: Pediatric Tumors.
Lyon, France: IARC; 2021
- Mazzola M, Bertoglio C, Achilli P et al.
Pancreatic ganglioneuroma: a rare entity with a
difficult
approach: a case report and systematic review. Dig
Med Res 2019;2:35
- Shaheen AA, Gill I, Edhi AI, Amin M, Cappell
MS. Pancreatic Ganglioneuroma Presenting in an
Octogenarian. ACG Case Rep J. 2021 Mar
19;8(3):e00546. doi:
10.14309/crj.0000000000000546.
- Poves I, Burdío F, Iglesias M,
Martínez-Serrano Mde L, Aguilar G, Grande L.
Resection of the uncinate process of the
pancreas due to a ganglioneuroma. World J
Gastroenterol. 2009 Sep 14;15(34):4334-8.
doi: 10.3748/wjg.15.4334.
- Ikoma N, Santamaria-Barria JA, Wray C, Tsao K.
Ganglioneuroma of the pancreas in a 4-year-old
girl. BMJ Case Rep. 2016 Nov
14;2016:bcr2016217425. doi:
10.1136/bcr-2016-217425.
- Christein JD, Kim AW, Golshan MA, Maxhimer J,
Deziel DJ, Prinz RA. Central pancreatectomy for
the resection of benign or low malignant
potential neoplasms. World J Surg. 2003
May;27(5):595-8. doi: 10.1007/s00268-003-6848-4.
- Yildirim O, Ozgen KH, Alkhatalin M, Elwakil M,
Camurdan VB. Pancreatic ganglioneuroma in a
young female. Rep Pract Oncol Radiother. 2022
Oct 31;27(5):929-930. doi:
10.5603/RPOR.a2022.0095.
- Domanski HA. Fine-needle aspiration of
ganglioneuroma. Diagn Cytopathol. 2005
Jun;32(6):363-6. doi: 10.1002/dc.20269.
- Scandavini C, Valente R, Rangelova E et al.
Pancreatectomies for pancreatic neoplasms in
pediatric and adolescent age: A single
institution experience. Pancreatology.
2018 Mar;18(2):204-207. doi:
10.1016/j.pan.2017.12.009.
- Avila-Sanchez P, Barron-Cervantes NM,
Martinez-Esteban A, Chan-Nuñez LC.
Retroperitoneal Peripancreatic Ganglioneuroma
Encasing the Celiac Trunk and Superior
Mesenteric Artery. Cureus. 2024 Jan
16;16(1):e52405. doi: 10.7759/cureus.52405.
|



















