|
Introduction
Occupational
mental health is an essential aspect of overall
well-being, impacting individuals, broader
workforce and workplace productivity. In India, as
in many other countries, there is a growing
recognition of the importance of mental health at
work. As per S&P Global Ratings, the Indian
economy, the fastest-growing among major
economies, grew at 7.2% in 2022-23 and is likely
to grow at 6.7% for the next three years(1). As a
fast-growing economy with a diverse and rapidly
changing work environment, India faces several
challenges and opportunities in promoting
occupational mental health. The World Health
Organization suggests that the worldwide economy
loses approximately 1 trillion dollars in
productivity each year due to mental health
issues(2). Another WHO forecast predicts economic
losses related to mental health conditions to
reach approximately dollar 1.03 trillion between
2012 and 2030 in India alone(3).
Characterized by
rapid industrialization, urbanization, and
technological advancement, occupational mental
health space in fast-developing economies presents
unique challenges driven by rapid economic growth,
cultural factors, and changing work dynamics.
Addressing these issues requires a comprehensive
and culturally sensitive approach, involving
governments, employers, and healthcare providers
to ensure the well-being of the workforce.
Occupational mental health in India is a serious
issue, with a substantial body of literature
highlighting wide prevalence of workplace-related
stress.
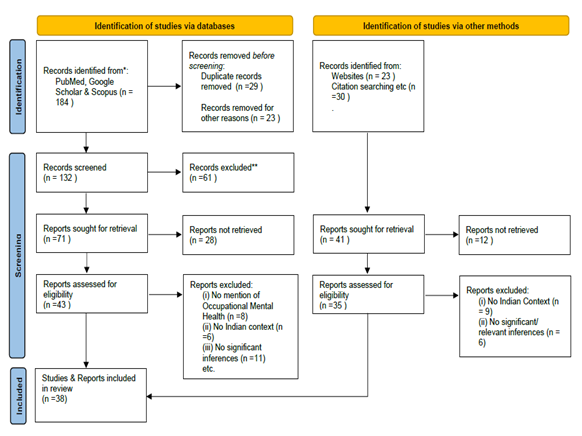
Methodology:
A comprehensive
review of the literature was carried out by
initially searching for related studies and topics
across various databases, predominantly from
PubMed, Google Scholar, Scopus, and websites. The
subjects covered the common occupational mental
issues in the fast-developing economy countries,
Occupational mental health scenario, the existing
interventions and the suggested remedial/ policy
measures specifically in Indian workspace. A total
of 237 records were reviewed. Among these, 37
duplicate records were removed, and 138 records
that didn't pertain to the study, for instance,
those unrelated to mental health, occupational
workers, or specific to the Indian or fast
developing economy context, were excluded.
Finally, the most pertinent 38 works were included
in this review. It is important to note that
academic work on similar lines in disadvantaged
section of the workforce viz. unorganized sector
is not readily available. Barring few, almost all
literature in peer reviewed journals is available
from more urban background, organized background
or industry background. Literature on mental
health issues and stress in healthcare workers is
a treatise in itself and therefore has not been
included in the subsequent discussion.
|
| Fig.1:
Prisma(4) Flow Diagram of the Study |
The Common Mental Issues
with the Fast-Developing Economies:
Work
Intensity and Pressure:
Researchers have
explained that the intensity of work is one of the
major dimensions deciding job quality. It is sin
qua non that a manageable intensity of work and
emphasising its implications for physical and
mental health, as well as for opportunities to
have a satisfying personal and family life.(5)
Fast-developing economies often witness increased
work intensity and pressure due to the demands of
economic growth and globalization. This can lead
to high levels of stress and burnout among
workers(6). For instance, in China, the concept
where employees are expected to work from 9 a.m.
to 9 p.m., six days a week, commonly known as
"996" work culture, has garnered attention for its
detrimental effects on mental health(7). The
demands placed on employees to consistently excel
can create excessive stress, resulting in
heightened workloads, extended hours, increased
anxiety, and emotional burnout. In the absence of
adequate support, mental disorders and other
mental health issues can have a detrimental impact
on an individual's self-esteem, work performance,
attendance, and their ability to secure or
maintain employment. Depression and anxiety alone
result in the loss of a staggering twelve billion
working days annually
Employment
Uncertainties:
The gig economy,
where temporary roles are prevalent, and companies
engage independent workers for brief projects
within a free-market framework, is fast expanding
phenomenon of most developing economies. As per a
Boston Consulting Group report, India boasts a gig
workforce of 15 million individuals, active across
sectors like software, shared services, and
professional services and holds the fifth position
globally in flexible staffing, trailing behind
only the US, China, Brazil, and Japan(8).
Precarious employment, characterized by job
insecurity and lack of social protections, can
contribute to anxiety and depression.(9). Studies
do show an impact of employment uncertainty on
mental health. Job uncertainty and psychological
distress goes hand in hand to affect the value or
the image of the employee organisation
proportionally(10).
Technostress:
Technostress was
initially defined as a “modern disease of
adaptation caused by an inability to cope with the
new computer technologies in a healthy
manner”(11,12). It is now recognised as the
negative psychological relationship between people
and the introduction of new technologies as a
result of altered habits of work and collaboration
due to the use of modern information technologies
at office and home situations(8).The technostress
in fast-developing economies is leading to a
situation where employees feel overwhelmed by
constant connectivity and information overload due
to rapid adoption of technology and rapid
digitalization in workspace(13). In addition due
to digitization of many processes workers feel
susceptible to being replaced in case of
non-satisfactory work performance(14). This issue
is particularly pertinent in countries like India
and Brazil, which have seen a quick surge in
digitalization.
Cultural
Factors:
Cultural factors
influence understanding, presentation, diagnosis,
management, course and outcome of mental
illnesses. (15). Cultural factors, such as the
stigma associated with mental health issues
including the sexual orientation, play a
significant role in fast-developing economies. In
many Asian countries, there is a reluctance to
discuss mental health problems openly, which can
hinder early intervention(16). Along with social
stigma attached with mental health problems and
their treatments, low levels of awareness and lack
of support from peers hamper timely and proper
help-seeking in India(17). It may come in the way
of the employee with a mental health condition
from seeking timely help or none at all. This can
lead to further deterioration, depression, loss of
self-esteem and other poorer psychosomatic health
outcomes. Furthermore, this stigma of being a
mental or psychological case, may lead workers to
hide or ignore risks to their mental health for
the fear of negative consequences in the
workplace, such as differential treatment or loss
of job. Cultural sensitivity is crucial when
designing mental health programs.
Inadequate
Occupational Health Services:
Many fast-developing
economies face challenges in providing accessible
and effective occupational health services. This
can limit the availability of mental health
support for workers(18). Strengthening healthcare
infrastructure is vital for addressing mental
health issues. A holistic approach or the total
worker health concept for the employee wellness
has occupational mental health as one of the core
ingredients is still catching up in developing
economies(19). Workers in these countries often
have to cope-up with the workplaces that have poor
overall health and safety policies, poor employer
employee communications and management policies,
and no or negligible mental well-being programs
which may affect their mental health adversely.
For numerous decades, both international and
national laws have been established to safeguard
the human rights of employees in the workplace.
Despite this, the implementation of these policies
varies and frequently falls short of being
optimal. Additionally, in low- and middle-income
countries—where the largest working-age population
resides—there remains a persistent lag in
executing or identifying appropriate
interventions. Furthermore, these regions often
lack sufficient policies to prevent discrimination
against employees dealing with mental
disorders(20,21).
The Indian Occupational
Mental Health Scenario:
The prevalence of
mental health issues in the Indian workforce is a
growing concern. India’s workforce comprises
nearly 92 per cent in the unorganised segment,
with the entire farm sector falling under the
informal category, while only one-fifth of the
non-farm workers are found in the organised
segment.(22) Numerous studies and surveys have
documented the high prevalence of occupational
stress and mental health issues among Indian
workers. According to a study conducted by global
consulting firm McKinsey, four out of every 10
working in corporate India are showing high levels
of burnout, distress, anxiety, and depression(23).
Literature reviews do indicate the impact of
stress in the post COVID period(24). Deadlines,
burdensome and demanding workloads, poor team
cultures, lack of recognition, and poor job
satisfaction were found to be the usual
contributors. Job insecurity, poor work life
balance, gender bias, poor workplace mental health
services, cultural factors including stigma
attached with mental illness, and peer pressure
are other significant factors impacting
occupational mental health in India. A
cross-sectional study encompassing 35 countries,
India included, reveals that approximately
two-thirds of employees experiencing depression
encountered discrimination either in their current
workplace or during job applications (20). Table 1
presents the number of references for leading
contributors to occupational mental health
disorders in India. Figure 2 depicts the same in
pie diagram. It may be noted that many references
had listed more than one contributor.
|
Table 1: Common contributors to
occupational mental health disorders in
Indian workplaces.
|
|
No.
|
Occupational mental Health Factors
|
No. of refs.
|
|
1.
|
Lack of recognition and poor job
satisfaction
|
9
|
|
2.
|
Job insecurity
|
18
|
|
3.
|
Deadline, demanding work pressure
|
4
|
|
4.
|
Poor work life balance
|
6
|
|
5.
|
Gender Bias, discrimination
|
5
|
|
6.
|
Stigma and cultural factors
|
5
|
|
7.
|
Work related stressors and precarious
work arrangements
|
4
|

|
| Fig.2:
Relative proportions of references of
major contributors to occupational mental
health disorders in Indian workplaces.
|
A Deloitte "Mental
health in the workspace 2022" survey, with 3,995
subjects across 12 key industries and demographics
found the workplace to be a top stressor, with 47
percent respondents undergoing workplace related
stress(25). It also concluded that the COVID-19
pandemic heightened and introduced new mental
health factors by obscuring the boundaries between
work and home, posing mental health challenges
such as longer work hours, the isolation
associated with virtual working environment, and
job security concerns. About 76% of Indian workers
indicate that stress has a negative impact on work
performance with 49% expressing similar sentiments
about their mental health, according to a survey
by ADP Research Institute(26)
Recent survey
studies in India revealed that more than a quarter
of Indian employees (36%) were experiencing mental
health problems, and half of the sample (50%) were
worried about job uncertainties(27). A study
conducted by ASSOCHAM in 2015 found that 43% of
employees in the private sector experienced signs
of general anxiety disorder or depression.(28) A
poll of 3000 corporate employees from 8 cities
across India and from 10 diverse sectors that
included e-commerce, FMCG & Hospitality, to
name a few, showed that 8 in 10 employees had
skipped work for a period of 14 days due to mental
fatigue in the preceding year(29). The National
Mental Health Survey of India revealed that
workplace stress was a significant contributor to
mental health problems, affecting both urban and
rural employees(30). A study by Yardi and Adsule
found sleeping disorder in a group of corporate
workers (day shift) to be at 13.8%. Insomnia is a
known medical comorbidity with anxiety disorders,
depression and hypertension(31). Some have
reported that the prevalence of anxiety disorders
among Indian employees was around 21.1%, while the
prevalence of depression was 13.9%. Research has
emphasized the mental health challenges workers
face in the informal sector in India(32,33). These
findings highlight the substantial burden of
mental health conditions in the workplace.
Furthermore, stress and burnout are common among
Indian professionals, driven by factors such as
heavy workloads, job insecurity, and the pressure
to meet performance target. Studies in factory
workers elucidate a clear presence of multiple
psychiatric morbidities including substance use.
These groups also carry many associated risk
factors and psychosocial factors that increases
their vulnerability to poorer health
outcomes.(34,35). Authors have also reported need
for further research to get a complete picture of
the problem.
A study by Bhagat et
al. highlighted the detrimental impact of job
insecurity on the mental well-being of Indian IT
professionals. Several other determinants
contribute to the mental health challenges faced
by Indian workers.(36) Work-related stressors,
inadequate work-life balance, and a lack of social
support at the workplace have been identified as
significant factors. The nature of employment,
including precarious work arrangements and job
insecurity, also plays a role in the mental health
of workers. Gender disparities in the workplace
also have implications for occupational mental
health. Women in India often face workplace
harassment and discrimination, which can lead to
mental health problems. A study by Vartak et al.
(2019) examined the association between workplace
harassment and depression among female employees
in India and found it to be a significant concern.
A cross-sectional study spanning 35 countries,
including India, found that approximately
two-thirds of employees who experienced depression
encountered discrimination either within their
current workplace or during their job application
processes(20).
Additionally, the
stigma associated with mental health issues in
India can discourage individuals from seeking
help, further exacerbating the problem(34). Stigma
around mental illness remains a substantial
barrier to seeking help. Research by Raguram et
al. explored the impact of cultural factors on
mental health stigma and help-seeking
behavior(37). Another study brought out an
alarming statistic that stigma in India prevents
nearly 80 percent of afflicted persons from
receiving treatment(38,39). As per a study,
however, employee silence in India has been found
to be negatively related to job burnout in
contrast to Western countries where employee
silence was positively related to undesirable work
outcomes and relationship between employee silence
and job burnout was mediated by Emotional
Intelligence(40).
Existing
Interventions for the Occupational Mental health
issues in India:
Efforts have been
made to address occupational mental health issues
in India. Various interventions and policies have
been proposed and implemented to address mental
wellness in Indian workplaces. Companies are
increasingly implementing Employee Assistance
Programs (EAPs) and mental health awareness
campaigns. The Indian government has launched
initiatives like the National Mental Health
Program (NMHP) to promote mental well-being. To
address the mental health needs of the Indian
workforce, various interventions and policies have
been proposed and implemented. Workplace stress
management programs, employee assistance programs,
and mental health awareness campaigns are gaining
traction in the corporate sector(41,42). The
Mental Healthcare Act of 2017 is a significant
step forward, emphasizing the importance of mental
health rights and services, including at the
workplace(43). Acknowledging the pandemic's effect
on individuals' mental health and overall
well-being, the Indian government made it a
priority by allocating investments in the 2022
Union budget to improve access to quality mental
health counselling and also care services(44)
However, challenges remain in the effective
implementation of these policies and
interventions. A study by Sagar et al. highlighted
the need for a more comprehensive approach,
integrating mental health into occupational health
programs and ensuring accessibility to mental
health services for all workers, including those
in the informal sector(45).
It is also important
that mental health wellbeing mechanisms are
broadly aligned with the particular organization’s
policies(27). More careful observations and proper
feedback could help reduce the level of burnout
and increase job satisfaction and mental health
quality in certain professional segments(46).
Prominent Indian multinational corporations have
actively utilized the workplace to encourage
sustainable behavioural changes for long-term
mental health goals, resulting in tangible
benefits for the companies, their employees, and
the surrounding communities. These encompass
corporate wellness initiatives, such as work-life
balance strategies (like well-being-related
leaves, 'no meeting Fridays' policy, etc.),
wellness sessions including yoga, meditation, and
stress management. Additionally, they incorporate
employee assistance programs, such as outsourced
counselling services, mobile application-based
counselling, and a 24/7 telephone helpline.
Employee well-being programs encompass provisions
for physical healthcare services and mental health
services. Moreover, peer support programs involve
the availability of mental health advocates, peer
support, and peer-to-peer counselling.(47-49)
Unfortunately, there are no interventions or
systemic efforts for the employees’ mental
well-being in the unorganised sectors. In
Government establishment the mental well-being of
employees is mostly a neglected component of
overall occupational health curriculum of the
organisations.
It is essential to
recognize that cultural factors play a substantial
role in shaping the perception and management of
mental health issues in India. Stigma, family
expectations, and the influence of traditional
healing practices can impact an individual's
willingness to seek help(50) Tailored
interventions that consider these cultural nuances
are vital for the success of mental health
programs in India. Cultural and societal factors
play a significant role in shaping perceptions of
mental health in India. Despite extensive global
research on workplace stress, stigma, and
attitudes toward individuals facing stress or
mental health issues, along with the development
of interventions to address these issues more
effectively, this aspect remains significantly
overlooked across various industries and nations,
including India. However, only a small fraction of
the insights gained from these studies have been
put into practice(39,51).
Potential
Solutions and Future Directions:
Despite research and
the development of interventions aimed at
addressing workplace stress, stigma, and attitudes
toward employees dealing with stress or mental
illness, this aspect continues to be frequently
overlooked on a global scale, spanning various
industries and countries, India included, and only
a handful of the insights gained from these
efforts are effectively put into practice(39,51).
Moving forward, addressing occupational mental
health in India requires a multi-faceted approach.
It involves creating supportive work environments,
improving access to mental health services, and
raising awareness about mental health issues.
Addressing these issues requires a concerted
effort from various stakeholders such as
employers, policymakers, and mental health
professionals to create a healthier and more
supportive work environment(52). A concerted
approach for suicide prevention among younger
workforce in consonance with the prevailing
policies and programs is extremely warranted (53,
54). Biswas et al. in all in their small study
population comparing government and private sector
employees have noted that private sector jobs to
be more stressful in following domains viz. role
overload, role ambiguity, role conflict, poor
participation, powerlessness, intrinsic
improvement, low status and strenuous working
condition(55). There has been no systematic study
about the occupational workers in different
occupational settings except the big corporates
and to some extent the government sectors. Other
sectors such as, unorganised sector which employs
a very substantial percentage of total Indian
workforce, the government and public sector
undertakings and the small and micro, small and
medium enterprises. Small and medium-sized
enterprises (MSMEs) play a pivotal role in driving
economic growth within today's rapidly evolving
and dynamic business landscape. As these MSMEs
prepare to confront forthcoming challenges, it's
crucial to emphasize the importance of providing
mental health support and wellness programs for
their workforce(26).
Policymakers must
strive to enact labour reforms that protect
workers' rights, promote job security, and
regulate work hours in the unorganised and private
sectors. For example, China has started enforcing
labour laws to address the "996" culture(56).
Governments and organizations should invest in
expanding mental health services, ensuring that
they are accessible and affordable for all
workers(18). Employers should invest in mental
health awareness programs and training for
managers to recognize and support employees facing
mental health challenges(57). Establishing clear
policies on remote work and telecommuting can help
mitigate technostress and create a healthier
work-life balance (58).
As cultural factors
play a substantial role in management of mental
wellness in Indian workplaces, mental health
campaigns should be tailored to the cultural
context of the region to reduce stigma and
encourage help-seeking behaviour(59). Stigma,
family expectations, and the influence of
traditional healing practices can impact an
individual's willingness to seek help.(50)
Cultural sensitivity is vital when designing and
implementing mental wellness programs. Awareness
and information campaigns are required to enhance
trust, responsibility, enrolment, and active
engagement in existing programs(60).
Organizational social programmes, such as outings
and competitions, in addition to digital mental
health apps and technology have been proposed to
improve workplace mental well-being in Indian
scenario.
Conclusion
India faces unique
challenges in the realm of occupational mental
health due to a combination of various factors
that emanate from fast economic growth, rapid
industrialization and digitization, fast changing
employment patterns, and cultural factors. Several
occupational factors contribute to mental health
problems in India. Long working hours, job
insecurity, lack of work-life balance, and limited
access to mental health support services are
commonly cited issues with job insecurity as the
predominant contributor to the occupational mental
health cases in India. In Indian settings another
domain that cannot be disregarded is the stigma
towards mental illness which affects both initial
help seeking behavior and also leads to poor
compliance(61). Mental wellness in Indian
workplaces has been recently acknowledged as a
critical aspect of employee well-being that has
implications for both individuals and the broader
workforce. While there has been progress in
recognizing and addressing mental health concerns
in the workplace, there is still much work to be
done. A multi-layered approach that seeks to
improve the work culture and work environment to
make it more conducive for employees’ mental
wellbeing, easy and unhindered access to mental
health services, awareness and de-stigmatization
of mental and psychological disorders can go a
long way to improve the state of occupational
mental health in India. This however, requires
concerted and integrated efforts from all the
stakeholders including the policy makers,
employers, mental health professionals,
psychiatrists, and the labour organizations. It is
strongly recommended that sector specific
comprehensive mental health surveys across
unorganised, government and private sectors be
conducted to ascertain the wider extent of
occupational mental health in India so that
necessary interventions can be designed
accordingly and the corresponding policy tweaks,
if required, can be worked out.
Acknowledgement
The author is
grateful to Dr D.K. Aswal, Director, Health,
Safety & Environment Group, Bhabha Atomic
Research Centre, Mumbai for his keen interest and
guidance in this work.
Competing Interests: The
author declares no competing interests.
Funding: No
funding was obtained for this study.
Data Availability
Statement: The data that support the
findings of this study are available from the
corresponding author, [Vyom Saxena], upon
reasonable request.
References
- ET Bureau. India to be fastest-growing economy
for next three years: S&P Global Ratings -
The Economic Times [Internet]. [cited 2023 May
4]. Available from:
https://economictimes.indiatimes.com/news/economy/indicators/india-to-be-fastest-growing-economy-for-next-three-years-sp-global-ratings/articleshow/101276724.cms
- WHO. Mental health at work. WHO. Available
from: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/mental-health-in-the-workplace
- Birla N. Mental health may hurt India to tune
of $1.03 trillion; here’s a dose for cos. The
Economic Times. Sep 10, 2019
Available from: https://economictimes.indiatimes.com/magazines/panache/mental-health-may-hurt-india-to-tune-of-1-03-trillion-heres-a-dose-for-cos/articleshow/71045027.cms
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I,
Hoffmann TC, Mulrow CD, et al. The PRISMA 2020
statement: An updated guideline for reporting
systematic reviews. J Clin Epidemiol.
2021 Jun;134:178–89.
- Rubery J, Grimshaw D. The Organisation of
Employment: an international perspective. 2003.
Available from: https://research.manchester.ac.uk/en/publications/the-organisation-of-employment-an-international-perspective
- Hassard J, Teoh K, Visockaite G, Dewe P, Cox
T. The cost of work-related stress: a systematic
review. Journal of Occupational Health
Psychology. 2017 Mar 30;23.
- ANI. Toxic “996” work culture, China’s dark
side of labour exploitation. Available from: https://www.aninews.in/news/world/asia/toxic-996-work-culture-chinas-dark-side-of-labour-exploitation20211008172403/
- Sami L, Iffat R. Impact of Electronic Services
on Users: A Study. JLIS.it. 2010 Dec
1;1.
- Artazcoz L, Benach J, Borrell C, Cortès I.
Social inequalities in the impact of flexible
employment on different domains of psychosocial
health. J Epidemiol Community Health.
2005 Sep;59(9):761–7.
- Chen H, Li J, Li J, Bao J. Role of employee
loneliness, job uncertainty and psychological
distress in employee-based brand equity:
Mediating role of employee exhaustion. Frontiers
in Public Health. 2022;10. Available from:
https://www.frontiersin.org/articles/10.3389/fpubh.2022.941106
- Brod C. Technostress: The Human Cost of the
Computer Revolution. Addison-Wesley Publishing
Company, Reading, USA. 1984
- Atanasoff L, Venable MA. Technostress:
Implications for Adults in the Workforce. The
Career Development Quarterly. 2017;65(4):326–38.
- Tarafdar M, Cooper CL, Stich J-F. The
technostress trifecta - techno eustress, techno
distress and design: Theoretical directions and
an agenda for research. Info Systems J. 2019;
29: 6–42. Available from:
https://onlinelibrary.wiley.com/doi/abs/10.1111/isj.12169
- Asad MM, Erum D, Churi P, Moreno Guerrero AJ.
Effect of technostress on Psychological
well-being of post-graduate students: A
perspective and correlational study of Higher
Education Management. International Journal
of Information Management Data Insights. 2023
Apr 1;3(1):100149.
- Gautam S, Jain N. Indian culture and
psychiatry. Indian J Psychiatry. 2010
Jan;52(Suppl1):S309–13.
- Lee SA, Jobe MC, Mathis AA. Mental health
characteristics associated with dysfunctional
coronavirus anxiety. Psychol Med. 2021
Jun;51(8):1403–4.
- Sanghvi PB, Mehrotra S. Help-seeking for
mental health concerns: review of Indian
research and emergent insights. Journal of
Health Research. 2021 Jan 1;36(3):428–41.
- Braquehais MD, Vargas-Cáceres S, Gómez-Durán
E, Nieva G, Valero S, Casas M, et al. The impact
of the COVID-19 pandemic on the mental health of
healthcare professionals. QJM. 2020 Jul
1;hcaa207.
- NIOSH, CDC. About the Total Worker Health®
Approach. 2023. Available from: https://www.cdc.gov/niosh/twh/about/index.html
- Brouwers EPM, Mathijssen J, Van Bortel T,
Knifton L, Wahlbeck K, Van Audenhove C, et al.
Discrimination in the workplace, reported by
people with major depressive disorder: a
cross-sectional study in 35 countries. BMJ
Open. 2016 Feb 23;6(2):e009961.
- Nardodkar R, Pathare S, Ventriglio A,
Castaldelli-Maia J, Javate K, Torales J, et al.
Legal protection of the right to work and
employment for persons with mental health
problems: a review of legislation across the
world. International Review of Psychiatry. 2016
Aug 8;28:375–84.
- Sakthivel S, Joddar P. Unorganised Sector
Workforce in India: Trends, Patterns and Social
Security Coverage. Economic and Political
Weekly. 2006;41(21):2107–14.
- Sengupta D. Four in 10 in India Inc showing
high levels of burnout, anxiety, depression. Mint.
22 Aug, 2022. Available from: https://www.livemint.com/industry/four-in-10-in-india-inc-showing-high-levels-of-burnout-anxiety-depression-11661161465000.html
- Manchia M, Gathier AW, Yapici-Eser H, Schmidt
MV, de Quervain D, van Amelsvoort T, et al. The
impact of the prolonged COVID-19 pandemic on
stress resilience and mental health: A critical
review across waves. Eur
Neuropsychopharmacol. 2022 Feb;55:22–83.
- HRK News Bureau. 22% employees prefer not to
share their mental health issues at the
workplace. HR Katha. Sep 13, 2022.
Available from: https://www.hrkatha.com/research/22-employees-prefer-not-to-share-their-mental-health-issues-at-the-workplace/
- Bhattacharya R. 76% of Indian workers say
stress negatively impacting work, shows survey.
The Economic Times. Aug 17, 2023.
Available from: https://economictimes.indiatimes.com//jobs/hr-policies-trends/76-of-indian-workers-say-stress-negatively-impacting-work-shows-survey/articleshow/102810905.cms
- Pandya A, Khanal N, Upadhyaya M. Workplace
Mental Health Interventions in India: A Rapid
Systematic Scoping Review. Front Public
Health. 2022 May 3;10:800880.
- Shenoy J. Nearly 42.5% employees in private
sector suffer from general anxiety disorders:
Assocham Study. Times of India. April 6,
2015. Available from: https://timesofindia.indiatimes.com/city/mangaluru/nearly-42-5-employees-in-private-sector-suffer-from-general-anxiety-disorders-assocham-study/articleshow/46822843.cms
- Khatri K. Every second working professional is
prone to mental health issues: Survey. CNBCTV18.
10 May, 2023. Available from: https://www.cnbctv18.com/education/every-second-working-professional-is-prone-to-mental-health-issues-survey-16614461.htm
- Murthy RS. National mental health survey of
India 2015–2016. Indian Journal of
Psychiatry. 2017 Jan 1;59(1):21.
- Yardi N, Adsule S. A Cross-Sectional
Observational Study to Determine the Prevalence
of Insomnia amongst Indian Corporate Employees.
J Assoc Physicians India. 2015
Oct;63(10):20–5.
- Begum A, Shafaghi M, Adeel A. Impact of Job
Insecurity on Work–Life Balance during COVID-19
in India. Vision. 2022 Feb
3;09722629211073278.
- Rajesh IJ. The Level of Job Stress and Burnout
Across Employees of Six Sectors in Indian
Organizations. Journal of Organization and Human
Behaviour. 2016;5(2):29-36
- Mishra B, Kar N. Managing Work Related
Problems in Industries - The Need for Employee
Assistance Programmes. Indian Journal of
Occupational and Environmental Medicine.
2003 Jan 1;7:35–9.
- Chakrabarti A, Bhalla A, Dutta S. A profile of
substance abusers using the emergency services
in a tertiary care hospital in Sikkim. Indian
J Psychiatry. 2006;48(4):243.
- Bhagat DV. Job Insecurity and Emotional
Stability of Professionals at Their Work Place.
International Journal of Humanities and
Social Science Invention. October
2014;3(10):10-12.
- Raguram R, Weiss MG, Keval H, Channabasavanna
SM. Cultural dimensions of clinical depression
in Bangalore, India. Anthropology &
Medicine. 2001;8(1):31–46.
- Jyani G, Prinja S, Ambekar A, Bahuguna P,
Kumar R. Health impact and economic burden of
alcohol consumption in India. Int J Drug
Policy. 2019;69:34–42.
- Hanisch SE, Twomey CD, Szeto ACH, Birner UW,
Nowak D, Sabariego C. The effectiveness of
interventions targeting the stigma of mental
illness at the workplace: a systematic review. BMC
Psychiatry. 2016 Jan 6;16(1):1.
- Srivastava S, Jain AK, Sullivan S. Employee
silence and burnout in India: the mediating role
of emotional intelligence. Personnel Review.
2019 Jan 1;48(4):1045–60.
- Jain P, Batra A. Occupational Stress at
Workplace: Study of the Corporate Sector in
India. IOSR Journal of Business and
Management (IOSR-JBM) Jan. 2015;17(1.Ver.
III):13-21
- Lagrosen S, Lagrosen Y. Workplace stress and
health – the connection to quality management. Total
Quality Management & Business Excellence.
2022 Jan 2;33(1–2):113–26.
- Math SB, Basavaraju V, Harihara SN, Gowda GS,
Manjunatha N, Kumar CN, et al. Mental Healthcare
Act 2017 – Aspiration to action. Indian J
Psychiatry. 2019 Apr;61(Suppl 4):S660–6.
- Centre for Mental Health Law & Policy -
Keshav Desiraju India Mental Health Observatory
(IMHO). Budget for Mental Health: Analysis of
Union Budget 2022–2023. Available from: https://cmhlp.org/wp-content/uploads/2022/02/IMHO-Union-Budget-for-Mental-Health-2022-23-1.pdf
- Gupta S, Sagar R. National Mental Health
Programme-Optimism and Caution: A Narrative
Review. Indian Journal of Psychological
Medicine. 2018 Nov 1;40(6):509–16.
- Rana A, Soodan V. Effect of Occupational and
Personal Stress on Job Satisfaction, Burnout,
and Health: A Cross-Sectional Analysis of
College Teachers in Punjab, India. Indian J
Occup Environ Med. 2019;23(3):133–40.
- Seth M. Employee well-being trends and best
practices in the Indian IT industry. People
Matters. 11 June, 2021. Available from: https://www.peoplematters.in/article/wellness/employee-well-being-trends-and-best-practices-in-the-indian-it-industry-29640
- Cemazar SA. Employee Wellbeing in the
Workplace: Importance and Future Predictions. Semos
Cloud. 2020. Available from:
https://semoscloud.com/blog/employee-wellbeing/
- Truworth Wellness. Corporate Wellness Program
in India to Energize Your Population. Available
from: https://www.truworthwellness.com/corporate
- Khandelwal SK, Jhingan HP, Ramesh S, Gupta RK,
Srivastava VK. India mental health country
profile. Int Rev Psychiatry.
2004;16(1–2):126–41.
- Joyce S, Modini M, Christensen H, Mykletun A,
Bryant R, Mitchell PB, et al. Workplace
interventions for common mental disorders: a
systematic meta-review. Psychol Med.
2016 Mar;46(4):683–97.
- Ranade K, Kapoor A, Fernandes TN. Mental
health law, policy & program in India – A
fragmented narrative of change, contradictions
and possibilities. SSM - Mental Health.
2022 Dec 1;2:100174.
- Cherian AV, Lukose A, Rappai R, Vijaya Sagar
KJ, Armstrong G. Adolescent suicide in India:
Significance of public health prevention plan. Asian
J Psychiatr. 2020 Mar;49:101993.
- Vijayakumar L, Chandra PS, Kumar MS, Pathare
S, Banerjee D, Goswami T, et al. The national
suicide prevention strategy in India: context
and considerations for urgent action. The
Lancet Psychiatry. 2022 Feb 1;9(2):160–8.
- Biswas D. Initiatives By Tech Firms On
Employee Mental Health In India. Analytics India
Magazine. 12 October, 2021. Available from:
https://analyticsindiamag.com/initiatives-by-tech-firms-on-employee-mental-health-in-india/
- Wang JJ. How managers use culture and controls
to impose a ‘996’ work regime in China that
constitutes modern slavery. Account Finance.
2020;60: 4331-4359. Available from:
https://onlinelibrary.wiley.com/doi/abs/10.1111/acfi.12682
- Evans-Lacko S, Knapp M, McCrone P, Thornicroft
G, Mojtabai R. The Mental Health Consequences of
the Recession: Economic Hardship and Employment
of People with Mental Health Problems in 27
European Countries. PLOS ONE. 2013 Jul
26;8(7):e69792.
- Riedl R, Kindermann H, Auinger A, Javor A.
Technostress from a Neurobiological Perspective.
Bus Inf Syst Eng. 2012 Apr 1;4(2):61–9.
- Patel V, Saxena S, Lund C, Thornicroft G,
Baingana F, Bolton P, et al. The Lancet
Commission on global mental health and
sustainable development. Lancet. 2018
Oct 27;392(10157):1553–98.
- Samudre S, Shidhaye R, Ahuja S, Nanda S, Khan
A, Evans-Lacko S, et al. Service user
involvement for mental health system
strengthening in India: a qualitative study. BMC
Psychiatry. 2016 Jul 28;16:269.
- Hammarlund RA, Crapanzano KA, Luce L, Mulligan
LA, Ward KM. Review of the effects of
self-stigma and perceived social stigma on the
treatment-seeking decisions of individuals with
drug- and alcohol-use disorders. SAR. 2018
Nov;9:115–36.
|



















