|
Introduction
Chronic
suppurative otitis media (CSOM) is the most
commonly occurring disease affecting 6% of the
Indian population.1 CSOM is defined as
a chronic inflammatory process involving middle
ear cleft which includes epitympanum,
mesotympanum, hypotympanum, Eustachian tube, and
mastoid air cells.2 It is divided into
two groups: Safe or tubotympanic type and Unsafe
or atticoantral type. It is characterized by
chronic ear discharge and non-healing tympanic
membrane perforation and conductive deafness.
Conservative management is considered as the
initial treatment includes aural toilet, dry ear
precautions, topical or systemic antibiotics
according to culture and sensitivity results. If
these measures are ineffective, surgery is
necessary to obtain permanent dry ear, tympanic
membrane perforation closure with hearing
improvement.2
Myringoplasty
is a simple closure of tympanic membrane
perforation. Cortical mastoidectomy is clearing
the mastoid cavity disease and relieves the block
in the aditus and antral region thereby mastoid
aeration is achieved. Some factors are responsible
for the success or failure of ear surgeries. These
are categorized into two groups. Non-mastoid
factors include the age of the patient, Eustachian
tube function, site& size of the perforation,
ossicular status, and cochlear reserve and mastoid
factors include pneumatization and inflammation of
mastoid.3 Graft uptake and hearing
improvement depend on mastoid aeration.
Our retrospective
study is defined to compare the surgical outcome
of CSOM of safe type in patients who underwent
myringoplasty alone or with cortical mastoidectomy
with myringoplasty by assessing graft uptake and
improvement in pure tone audiometry values.
Materials and Methodology
A
retrospective study was conducted on 300 patients
who attended the Department of Otorhinolaryngology
at Chettinad Hospital and Research Institute.
Approval from the ethical committee was obtained.
All the patients were explained about the study
and informed consent was obtained. Patients
between the age group of 18-40 years belonging to
both sexes, CSOM of tubotympanic type with pure
conductive hearing loss were included in the
study. Patients with mixed or sensorineural
hearing loss, CSOM with cholesteatoma,
granulation, and revision surgery were excluded.
Detailed history
including symptoms and duration was taken.
Clinical examination including general and
systemic examination with thorough ENT examination
was carried out. The otoscopic examination was
done to define the size and site of tympanic
membrane perforation, middle ear status, and
Tunning fork test was performed. Pure tone
audiometry and x-ray mastoid were done.
Patients were
divided into 2 equal groups. Group I comprises 150
patients who underwent myringoplasty alone and
Group II comprises 150 patients who underwent
cortical mastoidectomy with myringoplasty.
Myringoplasty was done using temporalis fascia by
underlay technique. Both the group was assessed
for graft uptake and pure tone audiometry at one
month postoperative. Postoperative pure tone
audiometry values were compared with preoperative
values. The graft uptake rate and improvement in
the hearing were calculated and compared with both
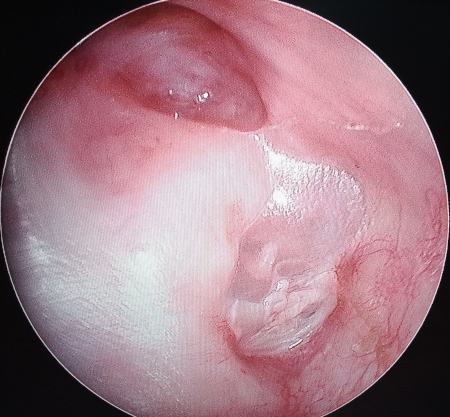
groups. The following images (obtained with
patient consent) Fig 1 and Fig 2 show patients
with chronic history of ear discharge and wet ears
with large perforation. These were included in
group II, Fig 3 shows image of a patient with
chronic otitis media having dry perforation and
was included in Group I.

|

|
| Fig
1: Otoendoscopy picture of patient with
chronic otitis media with central
perforation |
Fig
2: Otoendoscopy picture of patient with
chronic otitis media with repeated ear
discharge |

|
Fig 3: Otoendoscopy
picture of patient with chronic otitis
media having dry perforation |
Results
The mean age group is 30.627 and standard
deviation is 6.8442 (Table 1).
|
Table 1:
Descriptive Statistics
|
|
N
|
Minimum
|
Maximum
|
Mean
|
Std. Deviation
|
|
Age
|
300
|
19.0
|
40.0
|
30.627
|
6.8442
|
|
Valid N (listwise)
|
300
|
|
|
|
|
Patients were
divided into 2 equal groups. Group I comprises 150
patients (50%) who underwent myringoplasty alone
and Group II comprises 150 patients (50%) who
underwent cortical mastoidectomy with
myringoplasty (Table 2).
|
Table 2: Group
Distribution
|
|
Frequency
|
Percent
|
Valid Percent
|
Cumulative Percent
|
|
Valid
|
Myringoplasty
|
150
|
50.0
|
50.0
|
50.0
|
|
Myringoplasty with cortical
mastoidectomy
|
150
|
50.0
|
50.0
|
100.0
|
|
Total
|
300
|
100.0
|
100.0
|
|
Among 300 patients 148 patients (49.3%) were
male and 152 patients (50.7%) were female (Table
3) (Figure 1).
|
Table 3:
Sex-Wise Distribution
|
|
Frequency
|
Percent
|
Valid Percent
|
Cumulative Percent
|
|
Valid
|
Male
|
148
|
49.3
|
49.3
|
49.3
|
|
Female
|
152
|
50.7
|
50.7
|
100.0
|
|
Total
|
300
|
100.0
|
100.0
|
|
Among 300 patients
172 (57.3%) were employed and 128 (42.7%) were
unemployed (Table 4).
|
Table 4:
Occupation-Wise Distribution
|
|
Frequency
|
Percent
|
Valid Percent
|
Cumulative Percent
|
|
Valid
|
Employed
|
172
|
57.3
|
57.3
|
57.3
|
|
Unemployed
|
128
|
42.7
|
42.7
|
100.0
|
|
Total
|
300
|
100.0
|
100.0
|
|
Out of 300 patients
252 patients (84%) had hard of hearing and
remaining 48 patients (16%) had normal hearing
(Table 5) (Figure 2).
|
Table 5: Hard of
hearing
|
|
Frequency
|
Percent
|
Valid Percent
|
Cumulative Percent
|
|
Valid
|
Yes
|
252
|
84.0
|
84.0
|
84.0
|
|
No
|
48
|
16.0
|
16.0
|
100.0
|
|
Total
|
300
|
100.0
|
100.0
|
|
Out of 300 patients
the graft uptake was present in 272 patients
(90.7%) and graft uptake was absent in 28 patients
(9.3%) (Table 6).
|
Table 6: Graft
uptake
|
|
Frequency
|
Percent
|
Valid Percent
|
Cumulative Percent
|
|
Valid
|
Yes
|
272
|
90.7
|
90.7
|
90.7
|
|
No
|
28
|
9.3
|
9.3
|
100.0
|
|
Total
|
300
|
100.0
|
100.0
|
|
|
Table 7: Paired
Samples Statistics
|
|
Mean
|
N
|
Std. Deviation
|
Std. Error Mean
|
|
Pair 1
|
Pre PTA
|
40.829
|
300
|
7.9480
|
.4589
|
|
Post PTA
|
24.565
|
300
|
7.9941
|
.4615
|
It shows mean for
pre PTA and post PTA are 40.829 and 24.565
respectively. And standard deviation for pre PTA
and post PTA are 7.9480 and 7.9941 respectively
(Table 7).
|
Table 8: Paired
Samples Test
|
|
Paired Differences
|
t
|
df
|
Sig. (2-tailed)
|
|
Mean
|
Std. Deviation
|
Std. Error Mean
|
95% Confidence Interval
of the Difference
|
|
Lower
|
Upper
|
|
Pair 1
|
Pre PTA - Post PTA
|
16.2640
|
7.1772
|
.4144
|
15.4485
|
17.0795
|
39.249
|
299
|
.000
|
The above Table
represents t(299)=39.249 and the significant value
is 0.000 which is less than 0.05 at 95% confidence
interval. Therefore, there is significant
relationship between Pre PTA and Post PTA (Table
8).
Discussion
Chronic suppurative
otitis media of tubotympanic type is a common
disease of middle ear cleft involving all age
groups. The causes of CSOM include infection,
Eustachian tube dysfunction, allergy, and trauma.1
Paparella et al. suggested otitis media involves
different stages in a continuum of events in that
active and inactive stages are part of
otomastoiditis due to its connection between the
middle ear cavity and mastoid air cells.2
The definite management is myringoplasty with or
without cortical mastoidectomy to eliminate the
disease and reconstruction of the hearing
mechanism.3 Myringoplasty was first
described by Lonis Petit and mastoidectomy was
popularized by William House in 1959.4

|

|
| Fig
4: Mastoidectomy being performed
intraoperatively |
Fig
5:
Completed mastoidectomy intraoperatively |
Myringoplasty is a
repair of the perforation of the tympanic
membrane. Cortical mastoidectomy involves the
eradication of the source of infection in the
mastoid and improves pneumatization although it
has a risk of squamous epithelium ingrowth, injury
to vital structures like facial nerve and inner
ear structure. Aeration of the middle ear and
pressure regulation is achieved by the mastoid.5
Mastoid will act as infection nidus if there is a
failure to relieve the atticoantral block leading
to surgical failure.6 Fig 4 and Fig 5
show the intraoperative images when mastoidectomy
is performed.
Holmquist and
Bergstrom's study from 1978 claimed that
mastoidectomy increased the likelihood that
patients with noncholesteatomatous chronic otitis
media would have a successful tympanoplasty.7
In study conducted by Methwani et
al, Graft uptake was 76.67% in tympanoplasty alone
group and 83.33% in tympanoplasty with cortical
mastoidectomy group. In the present study, pre-
and post-operative pure-tone average was compared
and the statistical difference between
tympanoplasty group and tympanoplasty combined
with cortical mastoidectomy group was
statistically significant.8
Pandey et al, study
showed the difference was significant (P<
0.05). The mean audiological assessment before was
38.12, after was 28.46 and benefit was 9.66 in
group I and 38.24, 26.4 and 11.84 respectively in
group II. The difference was significant (P<
0.05).9
The post-operative
hearing gain in Krishnan et al's study from 2002
was 75% in both groups.10 Similar to
this, Balyan et al. (1997) reported no significant
differences in graft failure rates or hearing
outcomes among 48 patients with CSOM who underwent
tympanoplasty with or without mastoidectomy. They
also agreed that the surgery had become more
difficult and dangerous because of the
mastoidectomy.11 A research published
in 2003 by Nayak et al. showed a success rate of
100% in mastoidectomy with tympanoplasty and 60%
in tympanoplasty of a sample size of 40 patients
who were monitored for a period of 20.4 months,
indicating that mastoidectomy is a successful
procedure.12
An analysis of 484
dry, post-infectious, unoperated,
noncholesteatomatous TM perforations by McGrew et
al. (2004) compared the effects of mastoidectomy
with canal wall up to tympanoplasty alone and
found that both groups experienced identical
perforation closure success rates of 91%.13
The utility of
tympanoplasty in chronic noncholesteatomatous
otitis media without mastoidectomy was similarly
supported by Mishiro et al. (2009), with an
equivalent rate of graft success and hearing
results regardless of the condition of the ear at
repair (draining vs. nondraining) or the addition
of a mastoidectomy.14
Tympanic membrane
perforation closure was successful in 76% patients
who underwent myringoplasty and in 78.3% of the 46
patients who underwent myringoplasty with
mastoidectomy, according to a research by Toros et
al. (2010). (p > 0.05) The difference in
hearing gain between the two groups was not
statistically significant.15,16
Most of the
previous studies showed that there is no
statically significant benefit in doing cortical
mastoidectomy in addition to myringoplasty. But
our present study showed cortical mastoidectomy
with myringoplasty gives better results when
compared to myringoplasty alone.
Post Operative
The patients in
both groups were assessed postoperatively for
status of graft uptake and for improvement in pure
tone audiogram. Results were better in Group II
where myringoplasty with cortical mastoidectomy
was done. These patients were followed every month
for 6 months and once in 3 months. The recurrence
of perforation and ear complaints were
considerably less in Group II. Fig 6 and Fig 7
show the post operative otoendoscopy images of
good graft uptake post mastoidectomy.

|
|
| Fig
6: Postoperative image intact
neotympanum |
Fig
7: Postoperative image of cortical
mastoidectomy and myringoplasty |
Conclusion
Our
retrospective study shows that there is a
statically significant difference in results in
both groups. The surgical outcome is better in
cortical mastoidectomy with myringoplasty. This is
with regard to graft uptake rate, improvement in
postoperative pure tone audiometry values, and
also improved pneumatization of mastoid. Thus,
through this study we can conclude that results of
cortical mastoidectomy with myringoplasty is
better than myringoplasty alone.
Strengths and Limitations
Our
study had a good number of participants and we
divided them equally into two groups. The results
obtained correspond with that of the population.
However our study did not include cases of
ossicular erosion,or attic perforations or
cholesteatoma which would require additional
middle ear work like ossiculoplasty, atticotomy,
modified radical mastoidectomy etc. So, we can
conclude that in cases of chronic suppurative
otitis media of tubotympanic type, doing a simple
cortical mastoidectomy to improve mastoid aeration
along with myringoplasty goes a really long way in
benefitting patients and improving the post
operative surgical outcome.
Consent
As per international standards or university
standards, participants’ written consent has been
collected and preserved by the author(s).
Ethical Approval
As per international standards or university
standards written ethical approval has been
collected and preserved by the author(s).
Competing Interests
Authors have declared that no competing
interests exist.
References
- Baz MR. Effect of cortical mastoidectomy on
audiological outcomes in mucosal chronic otitis
media. Al-Azhar International Medical
Journal. 2020 Mar 1;1(1):258-63.
- Paparella MM, Abdelhammid MM, Schachern PA,
Sahni R, Yoon TH, da Costa SS. Otopathologic
correlates of the continuum of otitis media. Annals
of Otology, Rhinology & Laryngology. 1990
Jun;99(6_suppl):17-22.
- Swamy DR, Shankar T, Kumar M. Role of cortical
mastoidectomy in myringoplasty: a clinical
study. Journal of Evolution of Medical and
Dental Sciences. 2016 Jul
11;5(55):3756-60.
- Martin MS, Raz Y. Mastoid surgery. In: Myers
EN (ed) Operative otolaryngology head and neck
surgery, Chap 115, 2nd edn. Elsevier, Amsterdam,
2008. pp 1163–1177.
- Kaur M, Singh B, Verma BS, Kaur G, Kataria G,
SinghS Kansal P, Bhatia B. Comparative
evaluation between tympanoplasty alone and
tympanoplasty combined with cortical
mastoidectomy in non cholesteatomatous chronic
suppurative otitis media in patients with
sclerotic bone. ISOR-JDMS. 2014
Jun;13(6):40-5.
- Bajaj AR, Sheikh S, Joshi S, Paike B. Benefit
of Tympanoplasty with or without Cortical
Mastoidectomy in Active Mucosal Otitis Media–A
Comparative Study. Bengal Journal of
Otolaryngology and Head Neck Surgery. 2019
Apr 30;27(1).
- Holmquist J, Bergstrom B. The mastoid air cell
system in ear surgery. Arch Otolaryngology.
1978;104:127-9.
- Methwani DA, Deshmukh PT. Comparative study of
type I tympanoplasty with or without
mastoidectomy in tubotympanic type of chronic
suppurative otitis media patients. Journal
of Datta Meghe Institute of Medical Sciences
University. 2017 Apr 1;12(2):85.
- Pandey S, Singh D, Singh BP, Sharma P. A
comparative study of tympanoplasty with or
without mastoidectomy in treatment of chronic
suppurative otitis media tubotympanic type.
International Journal of Health and Clinical
Research. 2020 Nov 30;3(10):132-5.
- Nagle SK, Jagade MV, Gandhi SR and Pawar PV.
Comparative study of outcome of type I
tympanoplasty in dry and wet ear. Indian J
Otolaryngol Head Neck Surg. April–June
2009; 61:138
- Krishnan A, Reddy EK, Nalinesha KM, Jagannath
PM. Tympanoplasty with or without cortical
mastoidectomy-a comparative study. Indian
Journal of Otolaryngology and Head and Neck
Surgery. 2002; 54(3): 195-198.
- Nayak DR, Balakrishnan R, Hazarika P, Mathew
PT. Role of cortical mastoidectomy in the
results of myringoplasty for dry tubotympanic
disease. Indian Journal of Otology.
2003; 9:11-5.
- McGrew BM, Jackson CG, Glasscock ME. Impact of
mastoidectomy on simple tympanic membrane
perforation. The Laryngoscope.
2004;114(3):506-511.
- Mishiro Y, Sakagami M, Takahashi Y et al: Long
term outcomes after tympanoplasty with or
without mastoidectomy for perforation in CSOM. Eur
Arch Otorhino Laryngol. 2009 Jun;
266(6):819-22.
- Gargava A, Verma P, Gupta A, Saxena S.
Comparative Study between Tympanoplasty vs.
Tympanomastoidectomy for the surgical outcome in
tubotympanic Type CSOM. International
Journal of Health and Clinical Research. 2021
Jun 16;4(11):179-81.
- Balyan FR, Celikkanat S, Aslan A, Taibah A,
Russo A, Sanna M. Mastoidectomy in
non-cholesteatomatous CSOM – is it necessary? Otolaryngol
Head and Neck. 1997;117(6):592-5.
|



















