|
Introduction
Adolescence
is a period of psychological and somatic growth
and development that spans between the ages of 10
and 19 [1,2]. Adolescent pregnancy and childbirth
remain a public health problem [2,3], with medical
and cognitive risks associated with biological
immaturity, the social determinants of health and
the quality of the healthcare system [3,4]. These
risks include poor attendance at antenatal clinics
[3,5], prematurity [5,6], obstructed labour [7],
vaginal tears , puerperal psychosis [8],
pre-eclampsia and eclampsia [9], low birth weight
[9] and high neonatal mortality [10]. Rural areas
are more vulnerable than urban areas [4].
Caesarean section is the surgical intervention
that is constantly on the increase, especially in
urban areas [11–13], with rates ranging from 5.0%
to 42.8% [14], [15]. In Africa, the frequency of
caesarean section varies from 5.0% to 37.5% and
6.6% among adolescents [11,14,16]. There are
regional differences [15]. The main indications,
in all age groups, are maternal and foetal. The
impact on maternal and neonatal mortality is not
negligible, especially in Africa [17,18]. Age
under twenty favours caesarean section due to
fetal-pelvic disproportion [2,11,19]. For Ymelle et
al. [18] in Cameroon, caesarean sections in
adolescents represent 6.9%. Eouni et al.
[1] report 44% caesarean sections among teenage
deliveries in the Republic of Congo. In the
Democratic Republic of Congo, 11.7% of caesareans
in the town of Mbuji-Mayi were adolescents [20],
and the study conducted in the rural area of Moba
reported 48 cases of caesarean section among 523
deliveries of adolescents, i.e. 9.2% [2].
The aim of this
study is to determine the prevalence, indications,
evolution and factors associated with the risk of
caesarean section among adolescent in rural Lubao,
in the central-eastern Democratic Republic of
Congo. A comparison with adult women will enable
factors associated with the risk of caesarean
section to be determined.
Methods
Setting
This study was
conducted at the Lubao general referral hospital,
Lubao health zone and territory, Lomami province,
central Democratic Republic of Congo. The
territory of Lubao has three rural health zones
(Kamana, Tshofa and Lubao), each of which has a
general referral hospital, with no specialist
gynaecology and obstetrics doctor.
Type and
period of study
This was a
cross-sectional, analytical study with data
covering the period 2018 to 2022. The data were
collected by KoboCollect from the maternity ward
and operating theatre registers.
Inclusion criteria and sampling
For this study, we
included all deliveries during the data collection
period.
Data
collection
Data relating to
adolescents were obtained from partograms,
delivery registers and surgical operations
(caesarean sections). In some cases, operative
protocols were reviewed to complete the data on
vaginal deliveries. A KoboCollect data collection
form prepared in advance was used to collect the
variables sought on the adolescent girls and adult
women targeted by this study.
Operational definitions
Adolescent:
According to the WHO, this is a girl during the
age period between 10 and 19, i.e. less than
twenty years old.
Teenage
pregnancy: This is pregnancy that
occurs between the ages of 13 and 19.
Parameters
studied
a) Independent variable: Age
(years)
b)
Dependent variable: Frequency of
adolescent deliveries (by year of study),
occupation, level of education, marital status,
history of caesarean section, number of times
scarred uterus, parity, gestational age, modes of
delivery (vaginal and vaginal), type of pregnancy
(singleton and multiple), indication for caesarean
section, mode of admission (referred and
non-referred), types of caesarean section
(scheduled and urgent), fetal presentation
(breech, cephalic, transverse), onset of labour
(artificial, spontaneous), maternal outcome (good,
bad, death), outcome of the newborn during the
maternal early neonatal period (good, bad, death).
Data processing and
statistical analysis
The data collected
by KoboCollect during the study period were
downloaded onto an Excel spreadsheet (Microsoft,
USA, 2010) and imported for processing into
Epi-Info 7.1 (Center for Disease Control and
Prevention, Atlanta, USA, 2011) [21] and Jamovi
2.3.21 [22]. The results were presented in the
form of tables and graphs (Figures) including
numbers, proportions expressed as a percentage and
indicators of location (central tendencies: mean,
extremes, median) and dispersion (interquartile
range and standard deviation). The relationship
between the various parameters studied was
established using the p-value and the odd ratio at
the significance level p ≤ 0.05.
Ethics
The data for this
study were collected in strict compliance with
confidentiality and protocol. Authorisation had
been obtained from the authorities managing the
two health entities targeted by our study.
Results
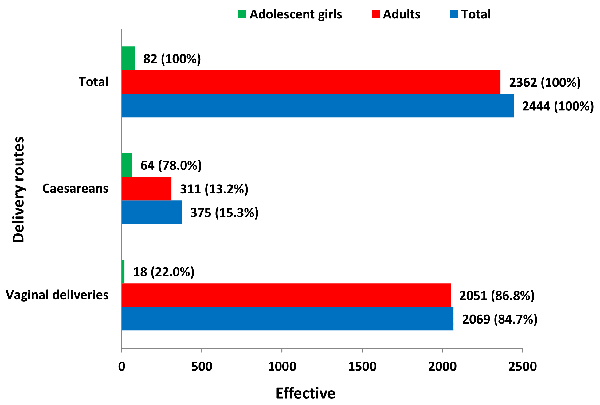
From 2018 to 2022,
2,444 deliveries were recorded at the Lubao
general referral hospital, including 375 caesarean
sections, or 15.3%. Among adolescent girls, 64
caesarean sections were performed out of 82
deliveries (78.0%), while adult women recorded
only 311 caesarean sections out of 2,362
deliveries (13.2%). The difference observed was
highly statistically significant (OR 23.44 [CI95%
13.71-40.09]; p=0.0000) (Figure 1).
|
Figure
1: Delivery routes at Lubao General
Referral Hospital
(p=0.0000; OR 23.448; IC95% 13.71-40.09) |
The typical profile
of the adolescent and adult woman shows that the
age varies from 15 to 19 years Vs 20 to 48 years,
with a median of 18 ± 0.25 years Vs 30 ± 12.5
years; student (n=43 i.e. 67.2% Vs n=6 i.e. 1.9%)
or farmer (n=19 i.e. 29.7% Vs n=160 i.e. 51.4%);
secondary education (n=62 or 96.9% Vs n=266 or
85.5%); married (n=50 or 78.1% Vs n=309 or 99.4%);
located less than six kilometers from the general
referral hospital (n=36 or 56.2% Vs n=194 or
62.4%). The differences observed between the two
groups were statistically significant for
occupation (p=0.0000), level of education
(p=0.0139) and marital status (p=0.0000) (Tables 1
and 3). There was no difference in the distance
travelled from home to the general referral
hospital (p=0.40803): the average was 9.95 ± 9.72
kilometers for adolescent girls and 8.3 ± 8.6
kilometers for adult women (Table 3).
|
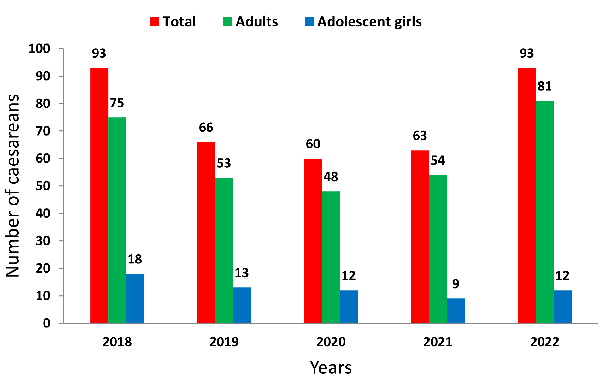
| Figure
2: Annual evolution of caesareans
|
Fetal macrosomia
(n=36; 56.3%), acute fetal distress (n=15; 23.4%)
and bony dystocia (n=7; 10.9%) were the main
indications for caesarean section among adolescent
women. Adult women in Lubao had fetal macrosomia
(n=86; 27.7%), acute fetal distress (n=78; 25.1%)
and placenta praevia (n=61; 19.6%) as the main
indications for caesarean section.
Mechanical dystocia
were predominantly encountered among adolescent
women, compared with dynamic dystocia in the group
of adult women. The difference observed was
statistically significant (OR 2.08 [IC95%
1.11-3.87]; p=0.0190) (Tables 2 and 4).
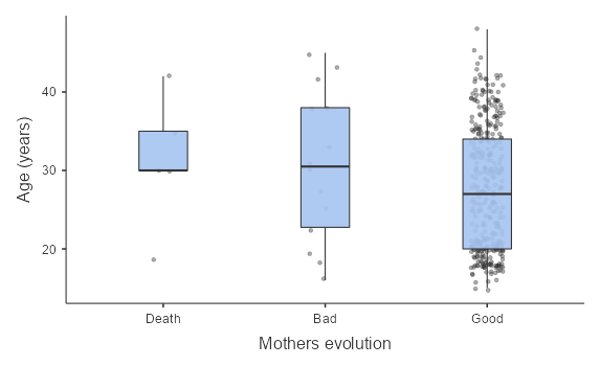
The maternal
outcome of caesareans was characterized by five
deaths (1.3%) and 14 poor outcomes (3.7%),
compared with 365 good outcomes (94.9%). Among
adolescents and adult women: one death (1.6%) Vs.
4 deaths (1.3%), three poor outcomes (4.7%) Vs 11
(3.5%) and 60 good outcomes (93.7%) Vs. 296
(95.2%). The difference observed was not
statistically significant (OR 1.31 (IC95%
0.42-4.10); p=0.6355). (Figure 3a)
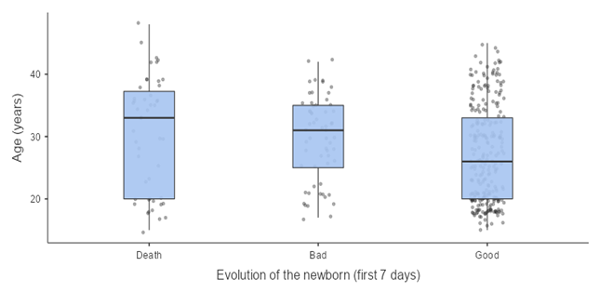
In the early
neonatal period, there were 49 deaths, 64 poor
outcomes and 277 good outcomes among the 390
newborns (360 singleton pregnancies and 15 twin
pregnancies). For adolescents and adult women
respectively: 9 deaths (14%) vs. 40 (12.9%), 6
poor outcomes (9.4%) vs. 58 (18.6%) and 49 good
outcomes (76.6%) vs. 228 (73.3). The difference
observed was not statistically significant (OR
1.40 (IC95% 0.75-2.62); p=0.3589). (Figure 3b).
Level of education did not influence maternal
outcome [OR 0.276 (95% CI 0.09-0.81); p=0.0136].
| Table
1: Sociodemographic characteristics
|
|
Characteristics
|
Total
|
Adolescents
|
Adults
|
p-value
|
|
Age (Years)
|
|
10-19
|
64 (17.1)
|
64 (100)
|
0
|
|
|
20 and over
|
311 (82.9)
|
0
|
311 (100)
|
0.0000
|
|
Extremes
|
15-48
|
15-19
|
20-48
|
|
|
Median + Interquartile
|
27 ±14.5
|
18 ± 0.25
|
30±12.5
|
|
|
Profession
|
|
None
|
120 (32.0)
|
1 (1.6)
|
119 (38.3)
|
|
|
Farmer
|
179 (47.7)
|
19 (29.7)
|
160 (51.4)
|
|
|
Pupil
|
49 (13.1)
|
43 (67.2)
|
6 (1.9)
|
0.0000
|
|
Trader
|
22 (5.9)
|
1 (1.6)
|
21 (6.8)
|
|
|
State public agent
|
5 (1.3)
|
0
|
5 (1.6)
|
|
|
Studies
|
|
Primary
|
36 (9.6)
|
1 (1.6)
|
35 (11.3)
|
|
|
Secondary
|
328 (87.5)
|
62 (96.9)
|
266 (85.5)
|
|
|
Higher and university studies
|
10 (2.7)
|
0
|
10 (3.2)
|
0.0139
|
|
Informal training
|
1 (0.3)
|
1 (1.6)
|
0
|
|
|
Marital status
|
|
Single
|
16 (4.3)
|
14 (21.9)
|
2 (0.6)
|
0.0000
|
|
Married
|
359 (95.7)
|
50 (78.1)
|
309 (99.4)
|
|
|
Distance from home to Hospital
|
|
≤ 5 Km
|
230 (61.3)
|
36 (56.2)
|
194 (62.4)
|
|
|
6 – 10 Km
|
16 (4.3)
|
3 (4.7)
|
13 (4.2)
|
0.40803
|
|
11 and over
|
129 (34.4)
|
25 (39.1)
|
104 (33.4)
|
|
|
Means + SD
|
|
9.95 ± 9.72
|
8.3 ± 8.6
|
|
|
Median + Interquartile
|
|
5.0 ± 16.8
|
4 ± 12
|
|
|
Extremes
|
1-40
|
1-38
|
1-40
|
|
| Table 2: Indications
for caesareans |
|
Indications
|
Total
|
Adolescents
|
Adults
|
|
Excess of term
|
5 (1.3)
|
0
|
5 (1.6)
|
|
Dystocia of presentation
|
20 (5.3)
|
3 (4.7)
|
17 (5.5)
|
|
Bone dystocia (borderline, shrunken
pelvis)
|
7 (1.9)
|
7 (10.9)
|
0
|
|
Failed uterine test (Dynamic dystocia)
|
18 (4.8)
|
0
|
18 (5.8)
|
|
Multiple pregnancy
|
15 (4.0)
|
0
|
15 (4.8)
|
|
Precious pregnancy
|
5 (1.3)
|
0
|
5 (1.6)
|
|
Fetal macrosomia
|
122 (32.5)
|
36 (56.3)
|
86 (27.7)
|
|
Placenta previa
|
61 (16.3)
|
0
|
61 (19.6)
|
|
Uterine rupture
|
4 (1.1)
|
1 (1.6)
|
3 (1.0)
|
|
Acute fetal distress
|
93 (24.8)
|
15 (23.4)
|
78 (25.1)
|
|
Scarred uterus
|
25 (6.7)
|
2 (3.1)
|
23 (7.4)
|
| Table 3: Obstetric
characteristics |
|
Characteristics
|
Total
|
Adolescents
|
Adults
|
p-value
|
|
Antecedents de caesarean
|
|
No
|
338 (90.1)
|
62 (96.9)
|
276 (88.7)
|
|
|
Yes
|
37 (9.9)
|
2 (3.1)
|
35 (11.3)
|
0.04704
|
|
Scarred uterus
|
|
No
|
338 (90.1)
|
62 (96.9)
|
276 (88.7)
|
|
|
Once
|
31 (8.3)
|
2 (3.1)
|
29 (9.3)
|
|
|
Twice
|
6 (1.6)
|
0
|
6 (1.9)
|
|
|
Gestational age (WA)
|
|
31-36
|
19 (5.1)
|
62 (96.9)
|
17 (5.5)
|
|
|
37-42
|
347 (92.5)
|
2 (3.1)
|
285 (91.6)
|
|
|
43 and over
|
9 (2.4)
|
0
|
9 (2.9)
|
|
|
Extremes
|
33 - 44
|
34 - 40
|
33 - 44
|
|
|
Means + SD
|
|
37. 6 ± 1.1
|
|
|
|
Median
|
|
37.0 ± 1.0
|
|
|
|
Parity
|
|
Nulliparous
|
114 (30.4)
|
46 (71.9)
|
68 (21.9)
|
|
|
Primiparous
|
94 (25.1)
|
18 (28.1)
|
76 (24.4)
|
0.0000
|
|
Pauciparous
|
87 (23.2)
|
0
|
87 (28.0)
|
|
|
Multipara
|
34 (9.1)
|
0
|
34 (10.9)
|
|
|
Grand multiparous
|
22 (5.9)
|
0
|
22 (7.1)
|
|
|
Types of pregnancy
|
|
Mono-fetale
|
360 (96.0)
|
64 (100)
|
296 (95.2)
|
0.149
|
|
Multifetale (twin)
|
15 (4.0)
|
0
|
15 (4.8)
|
|
|
Types of caesarean
|
|
Scheduled (elective)
|
13 (3.5)
|
1 (1.6)
|
12 (3.9)
|
0.5897
|
|
Urgent
|
362 (96.5)
|
63 (98.4)
|
299 (96.1)
|
|
|
Mode of admission
|
|
Refereed
|
240 (64.0)
|
39 (60.9)
|
201 (64.6)
|
0.5751
|
|
Not refereed
|
135 (36.0)
|
25 (39.1)
|
110 (35.4)
|
|
|
Beginning labor
|
|
Spontaneous
|
345 (92.0)
|
62 (96.9)
|
283 (91.0)
|
|
|
Artificial
|
30 (8.0)
|
2 (3.1)
|
28 (9.0)
|
0.114
|
|
Fetal presentation
|
|
Cephalic
|
348 (92.8)
|
59 (92.2)
|
289 (92.9)
|
|
|
Seat
|
15 (4.0)
|
3 (4.7)
|
12 (3.9)
|
0.968
|
|
Transverse
|
12 (3.2)
|
2 (3.1)
|
10 (3.2)
|
|
|
|
| Figure
3: Mothers (a) and new-born (b) evolutions
|
| Table 4:
Multivariate Analysis |
|
Characteristics
|
Total
|
Adolescents
|
Adults
|
OR
|
IC95%
|
p-value
|
|
Profession
|
|
Yes
|
255 (68.0)
|
63 (98.4)
|
192 (61.7)
|
39.04
|
5.34-285.27
|
0.0000*
|
|
Not
|
120 (32.0)
|
1 (1.6)
|
119 (38.3)
|
|
|
|
|
Secondary and over Studies
|
|
Yes
|
338 (90.1)
|
62 (96.9)
|
276 (88.8)
|
3.93
|
0.92-16.78
|
0.0477*
|
|
Not
|
37 (9.9)
|
2 (3.1)
|
35 (11.2)
|
|
|
|
|
Marital status
|
|
Single
|
16 (4.3)
|
14 (21.9)
|
2 (0.6)
|
43.26
|
9.54-196.10
|
0.0000*
|
|
Married
|
359 (95.7)
|
50 (78.1)
|
309 (99.4)
|
|
|
|
|
Distance: home to Hospital
|
|
≤ 10 Km
|
246 (65.6)
|
39 (60.9)
|
207 (66.6)
|
0.78
|
0.45-1.36
|
0.3887
|
|
11 and over Km
|
129 (34.4)
|
25 (39.1)
|
104 (33.4)
|
|
|
|
|
Antecedents of caesarean
|
|
No
|
338 (90.1)
|
62 (96.9)
|
276 (88.7)
|
3.93
|
0.92-16,78
|
0.0470*
|
|
Yes
|
37 (9.9)
|
2 (3.1)
|
35 (11.3)
|
|
|
|
|
Scarred uterus
|
|
Yes
|
36 (9.6)
|
2 (3.1)
|
34 (11.0)
|
0.26
|
0.06-1.11
|
0.0527
|
|
Not
|
338 (90.4)
|
62 (96.9)
|
276 (89.0)
|
|
|
|
|
Gestational age (WA)
|
|
31-36
|
19 (5.1)
|
2 (3.1)
|
17 (5.5)
|
0.55
|
0.08-2.47
|
0.4367
|
|
37-44
|
356 (94.9)
|
62 (96.9)
|
294 (94.5)
|
|
|
|
|
Parity ≤ 3
|
|
Yes
|
295 (78.7)
|
64 (100)
|
231 (74.3)
|
|
|
0.0000*
|
|
Not
|
80 (21.3)
|
0
|
80 (25.7)
|
|
|
|
|
Types of pregnancy
|
|
Mono-fetale
|
360 (96.0)
|
64 (100)
|
296 (95.2)
|
|
|
0.0729
|
|
Multifetale (twin)
|
15 (4.0)
|
0
|
15 (4.8)
|
|
|
|
|
Type of caesarean
|
|
Scheduled (elective)
|
13 (3.5)
|
1 (1.6)
|
12 (3.9)
|
0.39
|
0.05-3.09
|
0.360
|
|
Urgent
|
362 (96.5)
|
63 (98.4)
|
299 (96.1)
|
|
|
|
|
Mode of admission
|
|
Refereed
|
240 (64.0)
|
39 (60.9)
|
201 (64.6)
|
1.17
|
0.67-2.03
|
0.575
|
|
Not refereed
|
135 (36.0)
|
25 (39.1)
|
110 (35.4)
|
|
|
|
|
Beginning labor
|
|
Spontaneous
|
345 (92.0)
|
62 (96.9)
|
283 (91.0)
|
0.32
|
0.07-1.40
|
0.1144
|
|
Artificial
|
30 (8.0)
|
2 (3.1)
|
28 (9.0)
|
|
|
|
|
Fetal presentation
|
|
Cephalic
|
348 (92.8)
|
59 (92.2)
|
289 (92.9)
|
0.89
|
0.32-2.46
|
0.8351
|
|
No cephalic
|
27 (7.2)
|
5 (7.8)
|
22 (7.1)
|
|
|
|
|
Mechanical dystocia
|
|
Yes
|
239 (63.7)
|
49 (76.6)
|
190 (61.1)
|
2.08
|
1.11-3.87
|
0.0190*
|
|
Not
|
136 (36.3)
|
15 (23.4)
|
121 (38.9)
|
|
|
|
Discussion
Prevalence
of caesarean sections among adolescents
The persistent high
incidence of maternal deaths remains a challenge
for Africa and the Democratic Republic of Congo.
It is estimated that one woman in 42 is at risk of
maternal death, and 70% of maternal deaths are
attributable to Africa [15,23,24]. Preventable
causes, including those related to childbirth,
have been identified as the main causes of
maternal death [23].
Adolescent
childbirth spares no region of the World Health
Organisation [13,25–27]. In this series of
studies, we made a comparison with adult women in
order to determine the proportion of caesarean
sections in each group: the prevalence of
caesarean sections is scientifically higher among
adolescent girls than among adult women. These
results confirm what has been reported in the
medical literature in Guatemala, India, Kenya,
Pakistan, Zambia and the Democratic Republic of
Congo [26]. In Mbuji-Mayi, Claire et al. [20]
reported 11.7% of caesarean sections and John et
al. [28] 13.5% of caesarean sections among
adolescents, which is close to our results: 3.4%
of deliveries and 17.1% of caesarean sections. It
should be noted, however, that in studies on
caesarean section where the methodology does not
include a control group of adult women, there is a
risk of using the numbers of the majority of women
giving birth as a basis for wrongly concluding
that adult women present a higher risk of
caesarean section than adolescent women.
Precaution was used to avoid this risk of
interpretation bias.
Adolescents present
the risk associated with biological immaturity, as
demonstrated by the high risk of fetal-pelvic
disproportion and the numerous cases of
consequences associated with obstetric
inexperience [1,27].
Indications for caesarean section
The main indications
for caesarean section vary from region to region
[15]. In our study, caesarean sections were
significantly indicated for mechanical and
emergency dystocia. This may reflect the poor
quality of antenatal consultations. Fetal
macrosomia, acute fetal distress and bony dystocia
(found only among adolescents) are the main
indications for caesarean section among the
adolescents studied. These results are similar to
those reported by Adelaiye et al. [29]
except that pre-eclampsia/eclampsia replaces
macrosomia in first place. This predominance of
foetal macrosomia in adolescent and adult women
needs to be assessed. We are concerned about
diagnostic errors and recommend prospective and
KAP (knowledge, attitudes and practices) studies.
The majority of
studies on caesarean sections do not take controls
into account [7], [30], [31]. Comparative studies
of caesarean sections between adolescent and adult
women are still rare. We have not found a single
study conducted in our area (province) or in the
Democratic Republic of Congo.
Maternal and neonatal outcomes
Childbirth among
adolescents must be carefully monitored because of
the risks identified in the literature [7], [8],
[32], [33]. These risks can lead to maternal and
newborn deaths. In this study, overall maternal
mortality was 13‰ (five women) and early neonatal
mortality was 13.6% (49 newborns). It was found
that there was no statistical difference between
adolescent and adult women regarding maternal and
neonatal outcomes. Health care staff must improve
the quality of care for all categories of women
undergoing caesarean section, as the proportions
of maternal and newborn deaths remain high.
Vasconcelos et al. [34]recommend low APGAR scores
and the performance of resuscitation manoeuvres as
unfavourable factors in the outcome of newborns
born to adolescent mothers. In a meta-analysis,
Amjad et al. [4] mention low level of education as
a factor determining the unfavourable outcome of
pregnancy among adolescents, which is contrary to
our results. In our context, more in-depth studies
(integrating factors such as neonatal
resuscitation, maternal anaemia, birth weight, and
neonatal infection) are absolutely necessary to
evaluate the maternal outcome of caesarean section
and neonatal outcome between adult and adolescent
women.
Conclusion
Maternal and
neonatal mortality and morbidity remain a concern
for healthcare professionals. Childbirth remains a
crucial period which, with quality care, could
reduce the high frequency of maternal deaths in
our environment. Pregnancy among minors is a
serious public health problem for adolescent
girls, despite the measures that have been put in
place to combat it. Teenage girls have a very high
risk of caesarean section compared with adult
women. The main indications are avoidable. Raising
parents' awareness of the risks of early marriage,
educating girls about sex education in schools,
churches and youth clubs, combating sexual
exploitation and abuse, and even sexual violence,
are all solutions that should be considered.
Maternity wards also need to be equipped with
neonatal resuscitation facilities to ensure that
newborn babies are properly cared for. Priority
should be given to incubators (of which there are
none in the maternity unit) for temperature
control.
This study opens up
the possibility of multicentre studies to assess
the impact of measures to combat the marriage of
under-age girls.
Conflict of Interest
The authors do not declare any conflicts of
interest in connection with this study. This study
was funded by the authors' own contributions.
References
- Eouani LEM, Mokoko JC, Itoua C, Iloki LH.
Childbirth in the Adolescent Female at the
General Hospital of Loandjili (Congo).
Open Journal of Obstetrics and Gynecology.
2018;8(12):1140–6.
- Kabemba BH, Alimasi YG, Ntambwe AM, Kalamba
ME, Kitenge FF, Nyongonyi OE, et al.
Adolescent Pregnancy and Delivery in the Rural
Areas of DR. Congo: A Cross-Sectional
Descriptive Study (2014 to 2016). Open
Access Library Journal. 2018;5(8).
- Amoadu M, Hagan D, Ansah EW. Adverse obstetric
and neonatal outcomes of adolescent pregnancies
in Africa: a scoping review. BMC Pregnancy
Childbirth. 2022;27;22:598.
- Amjad S, MacDonald I, Chambers T,
Osornio-Vargas A, Chandra S, Voaklander D, et
al. Social determinants of health and adverse
maternal and birth outcomes in adolescent
pregnancies: A systematic review and
meta-analysis. Paediatr Perinat Epidemiol.
2019;33(1):88–99.
- Uzunov AV, Secara DC, Constantin AE, Mehedintu
C, Cirstoiu MM. Difference between Preterm Birth
in Adolescent and Adult Patients. Maedica
(Bucur), 2022;17(4):789–94.
- Afulani PA, Altman M, Musana J, Sudhinaraset
M. Conceptualizing pathways linking women’s
empowerment and prematurity in developing
countries. BMC Pregnancy Childbirth.
2017 Nov 8;17(Suppl 2):338.
- Kabemba BH, Mongane TB, Kunda SK, Saturnin
LBJJ, Ayumba DL, Tube JK, et al.
Epidemiological Profile of Childbirth among
Primiparous Women in Rural Areas of Tanganyika
Province, Democratic Republic of Congo. Open
Access Library Journal. 2021;8(3):1–13.
- Poinso F, Samuellian JC, Delzenne V, Huiart L,
Sparrow JS, Rufo M. Dépressions du post-partum:
délimitation d’un groupe à haut risque dès la
maternité, évaluation prospective et relation
mère-bébé. La psychiatrie de l’enfant.
2001;44(2):379–413.
- Ngowa JDK, Kasia JM, Pisoh WD, Ngassam A, Noa
C. Obstetrical and Perinatal Outcomes of
Adolescent Pregnancies in Cameroon: A
Retrospective Cohort Study at the Yaoundé
General Hospital. Open Journal of Obstetrics
and Gynecology. 2015;5(2):88–93.
- Ochieng AM, Agardh A, Larsson M, Asamoah BO.
Survival patterns of neonates born to adolescent
mothers and the effect of pregnancy intentions
and marital status on newborn survival in Kenya,
Uganda, and Tanzania, 2014–2016. Glob
Health Action. 2022;15(1):1-17.
- Essiben F, Belinga E, Ndoua CN, Moukouri G,
Eman MM, Dohbit JS, et al. La
Césarienne en Milieu à Ressources Limitées :
Évolution de la Fréquence, des Indications et du
Pronostic à Dix Ans d’Intervalle. Health
Sci Dis. 2020;21(2). In
https://www.hsd-fmsb.org/index.php/hsd/article/view/1771
- Ganeriwal SA, Ryan GA, Purandare NC, Purandare
CN. Examining the role and relevance of the
critical analysis and comparison of cesarean
section rates in a changing world. Taiwan J
Obstet Gynecol. 2021;60(1):20–3.
- Harrison MS, Garces AL, Goudar SS, Saleem S,
Moore JL, Esamai F, et al. Cesarean
birth in the Global Network for Women’s and
Children’s Health Research: trends in
utilization, risk factors, and subgroups with
high cesarean birth rates. Reprod Health.
2020 Dec 17;17(Suppl 3):165.
- Betran AP, Ye J, Moller AB, Souza JP, Zhang J.
Trends and projections of caesarean section
rates: global and regional estimates. BMJ
Glob Health. 2021;6(6):e005671.
- Osayande I, Ogunyemi O, Gwacham-Anisiobi U,
Olaniran A, Yaya S, Banke-Thomas A. Prevalence,
indications, and complications of caesarean
section in health facilities across Nigeria: a
systematic review and meta-analysis. Reprod
Health. 2023;20(1):81.
- Ochieng Arunda M, Agardh A, Asamoah BO.
Cesarean delivery and associated socioeconomic
factors and neonatal survival outcome in Kenya
and Tanzania: analysis of national survey data.
Glob Health Action. 2020;13(1):1748403.
- Malonga FK, Mukuku O, Ngalula MT, Luhete PK,
Kakoma JB. External anthropometric measurement
and pelvimetry among nulliparous women in
Lubumbashi: risk factors and predictive score of
mechanical dystocia. Pan Afr Med J.
2018;31:69.
- Ymele FF, Nenwa IFW, Fouedjio JH, Fouelifa LD,
Enow RM. Pronostic Maternel et Périnatal de
l’Accouchement chez les Primipares Adolescentes
et Adultes à Yaoundé. Health Sci Dis.
2020;21(3). Available from:
http://www.hsd-fmsb.org/index.php/hsd/article/view/1870
- Nahaee J, Abbas-Alizadeh F, Mirghafourvand M,
Mohammad-Alizadeh-Charandabi S. Pre- and during-
labour predictors of dystocia in active phase of
labour: a case-control study. BMC
Pregnancy Childbirth. 2020;20(1):425.
- Claire BKM, Fortunat MM, John KM, Cibangu K,
Tshimanga K, Michel KN, et al.
Determinants of the Quality of the Cesarean
Section in Mbuji-Mayi City (Democratic Republic
of Congo). Open Access Library Journal. 2021;8(2).
Available from:
http://www.oalib.com/paper/5432975
- Dean AG, Arner TG, Sangam CG, Sunki GC,
Friedman R, Lantinga M, et al. (2011)
Epi InfoTM, a database and statistics program
for public health professionals, Centers
for Disease Control and Prevention,
Atlanta, Georgia, USA.
- The Jamovi project. Jamovi. (Version 2.3)
[Computer Software]. Retrieved from
https://www.jamovi.org. 2022.
- Dumont A. Réduire la mortalité maternelle dans
les pays en développement: quelles sont les
interventions efficaces? Revue de Médecine
Périnatale. 2017;9(1):7–14.
- Kalombo PM. Problématique des accouchements
dystociques au centre de santé maternel et
infantile(CSMI) de Lubao, en République
Démocratique du Congo [Problem of dystocic
childbirth at the maternal and infantile health
center (CSMI) of Lubao, Democratic Republic Of
the Congo]. Tanganyika Journal of
Sciences. 2022;2(1):17–24.
- Dal’Maso E, Rodrigues PRM, Ferreira MG,
Moreira NF, Muraro AP. Cesarean birth and risk
of obesity from birth to adolescence: A cohort
study. Birth. 2022;49(4):774–82.
- Harrison MS, Pasha O, Saleem S, Ali S, Chomba
E, Carlo WA, et al. A prospective
study of maternal, fetal and neonatal outcomes
in the setting of cesarean section in low- and
middle-income countries. Obstetricia et
Gynecologica Scandinavica.
2017;96:410–420
- Coelho SJDC, Simões VMF, Batista RFL, Ribeiro
CCC, Lamy ZC, Lamy-Filho F, et al.
Birth by cesarean section and mood disorders
among adolescents of a birth cohort study in
northern Brazil. Braz J Med Biol Res.
2021;54(1):e10285.
- John KM, Claire BKM, Cibangu K, Ntumba M,
Fleur MC, Tshimanga K, et al.
Predictive Factors of Childbirth by High in the
City of Mbujimayi (Democratic Republic of
Congo). Open Access Library Journal.
2019;6(12). Available from:
http://www.oalib.com/paper/5424214
- Adelaiye SM, Olusanya A, Onwuhafua PI.
Cesarean section in Ahmadu Bello University
Teaching Hospital Zaria, Nigeria: A five-year
appraisal. Trop J Obstet Gynaecol.
2017;34:34-8
- Allagoa DO, Oriji PC, Tekenah ES, Obagah L,
Ohaeri OS, Mbah KM, et al.
Caesarean Section in a Tertiary Hospital in
South-South, Nigeria: A 3-year Review. European
Journal of Medical and Health Sciences.
2021;3(2):122–7.
- Jombo S, Ossai C, Onwusulu D, Ilikannu S,
Fagbemi A. Feto-maternal outcomes of caesarean
delivery in Federal Medical Centre, Asaba: a two
year review. Afr Health Sci.
2022;22(1):172–9.
- Chill HH, Lipschuetz M, Atias E, Shimonovitz
T, Shveiky D, Karavani G. Obstetric anal
sphincter injury in adolescent mothers. BMC
Pregnancy Childbirth. 2021;21(1):564.
- Mboua BV, Essiben F, Nana LP et al. Devenir
Maternel et Néonatal après Césarienne dans Trois
Hôpitaux de la Ville de Maroua. Health Sci
Dis. 2022 ;23(3). Available from:
http://www.hsd-fmsb.org/index.php/hsd/article/view/3468
- Vasconcelos A, Bandeira N, Sousa S, Machado
MC, Pereira F. Adolescent pregnancy in Sao Tome
and Principe: are there different obstetric and
perinatal outcomes? BMC Pregnancy and
Childbirth. 2022;22(1):453.
|



















