|
Introduction
In
India, tuberculosis (TB) is a serious public
health concern with 2.42 million cases were
reported in 2022, an increase of 13% from 2021,
which indicates the highest number of cases ever
reported in a single nation.(1–8) The bacterium
that causes TB, Mycobacterium tuberculosis,
has undergone genetic mutations over time, leading
to drug resistance and the emergence of novel
variants that present significant obstacles to the
control or management of the TB
epidemic.(1,3,4,8–14) Drug-resistant tuberculosis
(DR-TB) is primarily classified into two
categories: multidrug-resistant TB (MTB) and
extensively drug-resistant
TB(XDR).(3–5,9,12,14–16) The MDR-TB refers to TB
strains that are resistant to at least two of the
most powerful first-line drugs, isoniazid and
rifampicin.(3,8,12,14) The patient with XDR-TB, on
the other hand, is resistant to isoniazid,
rifampicin, and at least three of the six main
classes of second-line drugs (e.g., aminoglycosides,
polypeptides, fluoroquinolones, thioamides,
cycloserines, and para-aminosalicylic acid).(12,15)
The India TB Report divides DR-TB into four
categories based on the type of drug resistance
(Fig. 1).(4,17) In India, the DR-TB cases have
risen from 2012 by 17402 to 91841 in 2022 (Fig.
2).(7) However the incidence of DR-TB incidence
has significantly increased since 2012, but get
slightly decline between the COVID-19 waves that
started in 2020 (72787 Cases) and 2021 (70787
cases) (Fig. 2).(7,18–21) Numerous factors,
including a history of TB treatment, limited
access to diagnostic and treatment facilities,
lost follow-up, co-infection with HIV infection,
subpar healthcare infrastructure, insufficient
funding for TB control programmes, and ineffective
policies and strategies, have been associated with
the emergence of DR-TB in India.(3,10,12,22,23)

|
| Fig
1: Different types of DR-TB are divided
into four categories, as described by the
India TB Report 2023. |

|
| Fig
2: Year-wise reported incidence of
different types of DR-TB in India. |
Demography and Drug-Resistant Tuberculosis
The prevalence of
DR-TB varies by region, age, and gender, according
to a several studies carried out in India among
various populations.(1,2,6,8,9,12–14,22–28) Men
are 3.5 times more likely than women to be exposed
to the risk of developing DR-TB because of their
frequent drinking and smoking habits. It has been
noted that DR-TB risk factors vary by
gender.(6,24,26–29) Additionally, Maharashtra,
Gujarat, and Uttar Pradesh accounted for 48% of
all cases of DR-TB in the country in 2022.(7) In
comparison to other age groups, DR-TB is becoming
more common in economically active age groups
(18–54 years).(1,6,8,9,14,16,22–29) As a result of
the drug regimen used to treat DR-TB being linked
to a higher risk of treatment failure, relapse,
and mortality, which manifests in higher rates of
morbidity and mortality and also reported to have
high risk of developing DR-TB, particularly in
young children and pregnant
women.(1,2,12,15,26,30) One of the main reasons
among children of pediatric age for the
development of DR-TB is close contact with DR-TB
patients. (6,7,13)
Poverty and drug
resistance are major interconnected challenges
that significantly impact the fight against TB in
India. Patients with DR-TB often belong to lower
or middle socioeconomic classes and face various
socio-economic challenges.(22–27,29) They are more
likely to be married, come from joint households
(i.e., with more than four individuals), and have
limited education, with the majority having only a
high school attainments.(22–27,29) These people
frequently live in crowded rural areas, use
traditional smoke appliances to cook (i.e., Chulha),
and work as labourers.(22–27,29) Their
socioeconomic status, combined with a lack of
knowledge about TB treatment, puts them at a
higher risk of developing DR-TB.(23,25–27,29)
Furthermore, poverty exacerbates the problem by
resulting in poor nutrition, overcrowding, and a
lack of education and awareness, all of which
weaken the immune system and increase
vulnerability to TB infection and the development
of DR-TB.(22–26,28,29)
Objective
The main goal of
this in-depth review study is to evaluate and
comprehend the DR-TB epidemic's precarious
situation. The goal of the study is to examine the
difficulties encountered across India, such as the
demographics of those affected, the methods used
for diagnosis and treatment, and the policies and
programmes currently in place for the control of
DR-TB. The present study also aims to offer
insightful information on the epidemiology of
DR-TB, efficient clinical management techniques,
and public health approaches for addressing the
burden of DR-TB in India.
Methodology
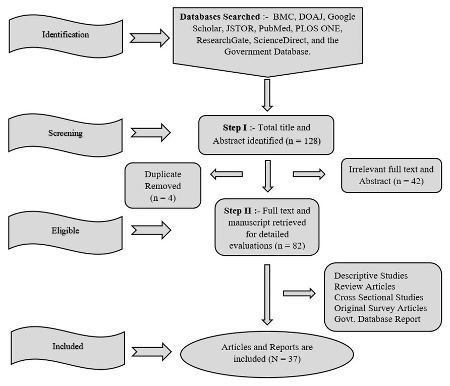
Utilizing a wide
range of international and national electronic
databases, including prestigious sources like BMC
journals, the Directory of Open Access Journals
(DOAJ), Google Scholar, JSTOR, PubMed, PLOS ONE,
ResearchGate, Science Direct, and the Government
Database, a thorough systematic diagnosis and
literature review were meticulously carried out.
The carefully selected search terms
"drug-resistant tuberculosis in India,"
"comorbidities associated with DR-TB," "treatment
challenges in DR-TB," and "DR-TB diagnosis
challenges" were used to ensure a thorough
examination of the literature that was already in
existence. Furthermore, pertinent technical
reports and government databases were carefully
identified and assessed while strictly adhering to
predetermined inclusion criteria to uphold the
results' integrity and reduce bias (Fig. 3). Also,
duplicate scientific papers yielded from different
search engines were excluded. The lengthy process
ended with the (N=37) downloading of the entire
manuscript, which included both the abstracts and
the full-length manuscripts. This allowed for the
interpretation, revision, and eventual completion
of this comprehensive review article.
|
| Fig
3: Steps to select the manuscripts and
complete this comprehensive review
article. |
Consequences of Drug-Resistant
Tuberculosis
Early TB detection
enables the development of an effective treatment
regimen, lowers the risk of future drug
resistance, and limits the
spread.(5,7,14,18–21,31) However, due to the
emergence of DR-TB, there are several problems
with treating TB, such as the cost of care, a lack
of diagnostic tools and laboratories, a higher
risk of transmission, newly identified M.
tuberculosis strains, ongoing mutations in
this bacteria, social stigma and discrimination,
social and economic issues, as well as other
related health issues.(2,8–10,12,28,30,32) The use
of additional therapies, such as second-line
therapies and injections, which are connected to
more detrimental side effects than conventional TB
treatment, is also one of the emerging causes of
DR-TB. (2,30) According to Shah et al. (2), Husain
et al. (30), and Kumar et al. (33), India
contributed to over one-fourth (26%) of the global
burden of DR-TB (in 2022), underscoring the
disease's rising prevalence and the difficulties
encountered in implementing the updated National
Strategic Plan, which aims to eradicate TB by
2025.(2,5,7,30,33) Contrarily, DR-TB therapy lasts
longer than 24–48 months compared to
drug-sensitive TB, making it more difficult, and
expensive for low- or middle-income families to
manage.(2,15,17,28,30,32) Due to the highly
contagious nature of DR-TB, patients must also be
isolated for longer periods of time. Additionally,
no close contacts should be present, as this could
increase the risk or vulnerability of the
situation.(15,17,28) The fact that patients and
caregivers experience social stigma and prejudice
while undergoing DR-TB therapy is one of the key
issues brought up by numerous research
investigation, primarily because of societal
misunderstandings, mistrust, misconceptions, and
myths.(2,12,28) The majority of DR-TB patients
experience social problems and feel helpless
because of their poor socioeconomic status and the
prolonged treatment of DR-TB, which exacerbates
their psychiatric comorbidities and makes
treatment more difficult.(15–17,28,29) The primary
causes of psychiatric comorbidities among DT-TB
are disease duration and literacy among the
vulnerable and caregivers.(28,32)
Comorbidities
associated with Drug-Resistant Tuberculosis
The TB epidemic with
associated comorbidities is vulnerable over time
and has challenging consequences and situations
for diagnosis and treatment, which eventually get
mutated into DR-TB.(1,15,16,28,29) Undernutrition,
HIV, diabetes, alcohol, and tobacco are major and
significant associated comorbidities among TB
patients that have a higher odds of emerging or
developing DR-TB.(1,15,16,28,29) These
comorbidities compromise the immune system,
increase the risk of treatment complications, and
contribute to the development of drug resistance.
In addition to the complexities of managing DR-TB,
patients suffering from comorbidities and vice
versa complicate overall health
outcomes.(1,15,16,28,29)
Undernutrition
Nutrient intake must
be appropriate to promote normal development,
growth, and overall health.(5,7,18–21) One of the
most pressing problems continues to be
undernutrition, which affects 663 million people
worldwide. (5) A few of the significant
contributors to undernutrition include poverty,
inadequate infant feeding and care practices, poor
maternal nutrition and health, and recurrent
illnesses.(5,7) Undernutrition is a significant
factor that amplifies the vulnerability of TB
patients to DR-TB and contributes to delayed
treatment, ultimately result in mortality. (1,14)
This is demonstrated by the fact that India ranked
107th out of 121 nations in the Global Hunger
Index in 2022. (5) Additionally, nutritional
deficiencies can lead to stunted growth, weakened
immune systems, cognitive impairments, and an
increased risk of TB.(1,14) Working with TB
patients during treatment is more challenging and
difficult because of undernutrition, which makes
it difficult for the body to maintain a strong
immune system.(1,7,14) It is difficult for the
National Tuberculosis Elimination Programme (NTEP)
to manage this dual burden in addition to the side
effects of DR-TB treatment because, according to
the India TB Report, a total of 7.38 lakh TB
patients are malnourished.(1,14) In a similar
vein, a large body of research indicates that
DR-TB is brought on by a number of factors, such
as weight loss, a BMI of less than 18.5 kg/m2,
a decrease in appetite, and issues with food
absorption during protracted and difficult TB
treatment. (1,7,14,27)
HIV
Human
immunodeficiency virus (HIV) is a major global
public health issue with 40 million cases
worldwide, where India ranks in third place with
24 lakh cases of people living with
HIV.(5,7,16,34) However, HIV is a causative agent
of acquired immune deficiency syndrome (AIDS),
which affects directly the body's immune system
and makes it prevalent to get sick from diseases
like TB, which is one of the most dreadful viruses
ever because there is no cure for HIV
infection.(5,15,16,25,26,29,31,35) The most common
way of transmitting HIV is through unprotected sex
or through the exchange of body fluids like blood,
breast milk, semen, and vaginal fluid.(5,7,16,35)
Conversely, HIV infection gets worse when it gets
associated with diseases like TB and increases the
risk of ramifications that lead to
DR-TB.(5,14,15,25,26,29,31,35) Several studies
revealed that HIV-TB infection is dominant in
males, with an average age group of about 30–40
years and a higher frequency of drug resistance
among HIV-TB
patients.(5,7,16,18–21,25,26,29,31,35) In 2022,
the India National AIDS Control Programme (NACP)
and the NTEP monitored 37578 total HIV/TB
cases.(7)
Alcohol
Worldwide, drinking
alcohol has caused major negative health effects
for decades and has become a common behavior and
way of life.(5,7,18–21) The National Family Health
Survey (NFHS-5, 2019-21) in India found that
alcohol usage has had a substantial impact on
people of all ages and genders, increasing
societal and personal problems, especially in
rural areas. In addition, there are 160 million
alcohol users in the country who consume billions
of liters of alcohol annually, with the percentage
of users continuously rising each year.(5,7,34)
Contrarily, numerous studies have shown that
alcohol use disorders and TB worsen the illnesses
and constitute a dual burden, which makes things
critical and more complicated over time by causing
mutation which increases morbidity and mortality,
and ultimately leading to DR-TB.(14,29)
Ramifications may occur for people with DR-TB who
continue drinking while receiving
treatment.(25,26,29) Additionally, due to a lack
of social support, divorced or widowed TB patients
are more likely to experience depression and
anxiety, which can lead to alcohol use. This makes
it even harder for them to adhere to treatment and
increases their risk of developing
DR-TB.(17,26,29,32) The dual burden of alcohol and
DR-TB causes a major hindrance in the direction of
diagnosis and treatment, and can lead to mutations
within M. tuberculosis, eventually
resulting in DR-TB. This, in turn, leads to
treatment complications and, potentially,
mortality.(10,14,17,26,29,32)
Diabetes
Diabetes is a
chronic, metabolic disease characterized by
elevated levels of blood glucose, which lead over
time to serious damage to the heart, blood
vessels, eyes, kidneys, and nerves.(5,26,29,36)
Globally, 422 million people have diabetes, of
whom India contributes 77 million adults, and 25
million are at high risk of developing
diabetes.(5,7,26) Diabetes compromises the immune
system, making individuals more susceptible to TB
infection and progression.(7,26,29,36) However,
the majority of people do not know or are ignorant
of their diabetes status, and those who had
concomitant diabetes during prior TB treatment
episodes had eight times greater odds of getting
DR-TB.(7,26,35,36) Additional delays in treatment,
prolonged exposure to anti-TB drugs, and impaired
immune responses among diabetes patients lead to
ramifications and mortality.(14,15,26,29)
Furthermore, managing such a dual burden among
individuals exacerbates health outcomes,
ultimately leading to increased rates of morbidity
and mortality.(16,36)
Tobacco
The coexistence of
tobacco use has emerged as a significant public
health concern, leading to 8 million deaths
worldwide annually, with India accounting for 1.35
million of these deaths.(5) Nicotine, a highly
addictive substance present in tobacco, represents
a substantial risk factor for infection from any
airborne disease.(5,7,29) Furthermore, tobacco use
and exposure to toxic second-hand smoke have a
higher risk of getting infected with TB,
progression from infection to active TB disease,
increased risk of recurrence and death from TB
globally, and eventually lead to substantial
social and economic costs.(26,29) According to the
India TB report (2023) in 2022, across India,
around 2,10,543 TB patients were identified as
tobacco users, with 67157 being linked with
tobacco cessation services.(7) However, a number
of studies revealed that the common cause of
worsening the vulnerability of TB patients and
spreading DR-TB was a history of residing in
places with second-hand smoke and past tobacco
use, whether it was chewing or smoking.(26,27,29)
Moreover, the dual burden of such a kind of
disease in public health concerns potentially
impacting treatment outcomes and increasing the
burden on healthcare systems.(5,7,18–21,26,27,29)
Diagnosis and Treatment of
Drug-Resistant Tuberculosis
In India, DR-TB is
rapidly increasing, and healthcare professionals
are facing significant difficulties in diagnosing
and treating DR-TB, which has serious
ramifications.(2,12,15,23,24,30,37) It is
challenging to monitor, manage, and regulate DR-TB
treatment in pediatric patients.(4,6,13,15) In the
DR-TB cases in children, the dosage of second-line
anti-tuberculosis drugs was based on the patient's
body weight.(13,15) Additionally, due to the
frequent and severe toxicity profile of
second-line drugs, female DR-TB patients of
reproductive age are at increased risk for harm to
both themselves and their fetus.(6,13,15)
The NTEP has
intended to expand the DR-TB diagnostic service
network, diagnosis tests, monitoring services, and
efforts of stakeholders to enhance health
outcomes, support quality-assured diagnostic
services, and provide a specific role in providing
ambulatory care for
patients.(3,7,8,11,15,18–21,24,28,33,37) India's
“Drug-Resistant TB Diagnostic Service Network"
includes the National Tuberculosis Reference
Laboratory, Intermediate Reference Laboratories,
private laboratories, and private and government
treatment centers.(7) Despite this support system,
the main difficulties faced by healthcare
professionals are a lack of modern laboratory
infrastructure, qualified staff, and appropriate
facilities for handling and processing specimens
particularly in rural areas.(2,37) In addition to
the DR-TB diagnosis network, DR-TB is frequently
diagnosed using culture-based techniques; however,
this process takes at least 12 weeks to
complete.(23,24,30) However, due to their cost and
limited availability of rapid molecular testing
techniques, are difficult to use in rural
areas.(15,23,24,30,37) Patients with DR-TB may
experience psychiatric comorbidities, such as
anxiety and depression, because of financial
strain, misconceptions, familial obligations, and
emotional distress.(17,28,32) Non-pharmacological
interventions, such as psychological and emotional
support, psycho-education, and methods like muscle
relaxation, mindfulness, and keeping a thought
journal, are given by caregivers, numerous
agencies, institutions, private and public
organizations, and health professionals to treat
these psychiatric comorbidities.(17,28,32)
Policy and programmatic
responses to Drug-Resistant Tuberculosis
The DR-TB is a
growing global health problem, with 27% of
infections coming from just one country: India.
DR-TB is already a pandemic in India because of
this frightening incident. Despite this, the
Indian government has implemented a variety of
targeted initiatives (Fig 4), treatments, and
policies to deal with the rising prevalence of
DR-TB in the nation.(3,7,8,15,24,28,33,37) These
include encouraging stakeholder engagement,
strengthening health systems, putting patient
support and social protection in place,
implementing infection prevention and control
measures, and encouraging research and
innovation.(7,28,33,37) The main aim of the Indian
government is the RNTCP, which is currently called
the NTEP.(15,33,37) To improve the management of
DR-TB, the NTEP devised the programmatic
management of DR-TB (PMDT), which focuses on early
detection, diagnosis, and appropriate treatment of
DR-TB cases.(3,7,8,15) Under the NTEP, India
established the largest TB laboratory network in
the world, enabling rapid diagnostic methods to
conduct universal drug susceptibility testing
(UDST) under one roof to quickly and affordably
diagnose DR-TB.(3,7,24,33) "Liquid Culture Media''
and "Nucleic Acid Amplification Test" (CABNAAT and
TrueNat) are these rapid diagnostic tests,
particularly for detecting pediatric, HIV-TB, and
EPTB. Moreover, the "Line Probe Assay" is a more
precise and quick molecular DST assay to diagnose
MDR and XDR-TB.(3,4,7,13)

|
| Fig
4: Implemented different schemes and
policy to reduce incidence of DR-TB under
NTEP in India |
The Direct Observed
Treatment Short Plus (DOTS) treatment scheme
(internationally recommended) calls for giving new
DR-TB patients supervision for a period of six
months to ensure that drug intake is being
monitored.(5,7,15,18–21,33) However, insufficient
data and a lack of intensive monitoring make the
situation vulnerable in the TB epidemic with
DR-TB.(15,33) Furthermore, new anti-TB drugs (e.g.
Bedaquiline, Delaminid and Linezolid)
with additional monitoring were made available for
the treatment of DR-TB and demonstrated a
significantly improved patient outcome.(1,8,37) In
addition, the Indian government launched a TB-free
campaign in order to reduce stigma and
discrimination, implement new healthcare
facilities (e.g., proper ventilation, use of
masks, and isolation of patients), provide
appropriate training to healthcare professionals,
and raise awareness regarding highly contagious
DR-TB. Even though the world is evolving, chronic
illnesses like DR-TB still necessitate lengthy
treatment regimens that may cause family
disruptions and an increase in dropout rates and
child labour.(27,29,37) To provide supportive
compression and reduce the occurrence of DR-TB in
low- and middle-income households in March 2018,
the Direct Benefit Transfer Schemes were
introduced.(37) In accordance with this, 500 INR
is sent in stages to the patient's bank account
each month to provide for proper dietary support
and, as a reward during treatment, transportation
allowances.(27,33,37) Additionally, the Indian
government has taken steps to improve access to
healthcare, particularly in rural areas, using a
public-private partnership strategy. It has
included the private sector in joint NTEP
initiatives to improve access to care and reduce
the TB epidemic with DR-TB.(7,33) Furthermore, a
real-time web-based surveillance system known as
"Nikshay" "NikshayAushadi," and the Lab
Information Management System were established as
part of the NSP in order to improve surveillance,
implement robust reporting, and effectively
monitor treatment.(3,7,33)
Future Challenges of
Drug-Resistant Tuberculosis
Future efforts by
the Indian government to control the TB epidemic,
particularly regarding DR-TB, will face
significant challenges due to the high percentage
of latent TB cases.(7,18–21,33) The emergence of
new DR-TB strains, which can result from mutations
in the M. tuberculosis bacteria as a
result of comorbidities and environmental factors,
will be one of the biggest challenges.
(4,5,7–10,14,15,23,24,30,37) Strong strategies
will be required to halt the highly contagious
nature of these new DR-TB strains.(3,5,12,14–16)
To enable the early and precise detection of DR-TB
cases with a patient-centered approach, ongoing
research and development initiatives, monitoring
and social support, investments in cutting-edge
diagnostic technologies, laboratory
infrastructure, and campaigning will be
necessary.(15,28) To improve treatment outcomes
for people with DR-TB in India, significant
funding will also be required.
Conclusion
The emergence of
DR-TB, which continues to be a global public
health concern, has made affected populations more
vulnerable. The Indian government must implement a
multifaceted, multi-sectoral strategy to
effectively combat this epidemic. This entails
making sure that there is an ongoing supply of
efficient medications, putting in place routine
monitoring and assessment mechanisms to spot gaps
in the healthcare system, and collaborating with
various stakeholders like government
organizations, pharmaceutical firms, and academic
institutions to ensure thorough reporting and
prompt treatment of all DR-TB patients.
Collaboration with non-governmental organizations
and private partners is also necessary to address
issues like patient education, stigma, and
restricted access to healthcare in remote and
underserved areas. Regular campaigns and the
planning of free medical camps can aid in bringing
attention to the issue and helping those in need.
By putting these suggestions into practice, the
Indian government can effectively combat DR-TB and
lessen its effects on public health.
Acknowledgement
The authors
gratefully acknowledge the help and cooperation of
the Department of Anthropology, Sikkim University.
The present review study was financially supported
in the form of the University Grants
Commission-Non-NET Fellowship, and Sikkim
University is also being acknowledged.
References
- Salhotra VS, Sachdeva KS, Kshirsagar N, Parmar
M, Ramachandran R, Padmapriyadarsini C, et al.
Effectiveness and safety of bedaquiline under
conditional access program for treatment of
drug-resistant tuberculosis in India: An interim
analysis. Indian Journal of Tuberculosis.
2020;67(1):29–37.
- Shah I, Poojari V, Meshram H. Multi-Drug
Resistant and Extensively-Drug Resistant
Tuberculosis. Indian J Pediatr.
2020;87(10):833–9.
- Singh N, Singh AK, Kumar S, Narendra Pratap
Singh NPS, Gaur V. Role of Mycobacterial Culture
and Drug Sensitivity Testing Laboratory under
National Tuberculosis Elimination Program for
the Abolition of Tuberculosis in India by 2025.
Journal of Clinical Diagnostic Research
[Internet]. 2022 [cited 2023 May 22]. Available
from: https://www.jcdr.net/articles/PDF/16655/55426_CE[Nik]_F(SHU)_PF1(AG_SS)_PFA(AG_KM)_PN(KM).pdf
- Khurana P, Saigal K, Ghosh A. Drug resistance
pattern and mutation pattern in pediatric
tuberculosis: Study from north India. Indian
J Tuberculosis 2021;68(4):481–4.
- WHO. Global tuberculosis report 2022
[Internet]. World Health Organization; 2022 Oct
[cited 2023 Jan 3] p. 68. Available from: https://www.who.int/publications/i/item/9789240061729
- Dhamnetiya D, Arora S, Jha RP. Tuberculosis
burden in India and its control from 1990 to
2019: Evidence from global burden of disease
study 2019. Indian Journal of Tuberculosis.
2023;70(1):87–98.
- India TB Report 2023 [Internet]. India:
Ministry of Health and Family Welfare Government
of India; 2023 [cited 2023 Jan 5] p. 296.
Available from: https://tbcindia.gov.in/showfile.php?lid=3680
- Resendiz-Galvan JE, Arora PR, Abdelwahab MT,
Udwadia ZF, Rodrigues C, Gupta A, et al.
Pharmacokinetic analysis of linezolid for
multidrug resistant tuberculosis at a tertiary
care centre in Mumbai, India. Front
Pharmacol. 2023;13:1081123.
- Jain A, Singh PK, Chooramani G, Dixit P,
Malhotra HS. Drug resistance and associated
genetic mutations among patients with suspected
MDR-TB in Uttar Pradesh, India. Int J
Tuberc and Lung Dis. 2016;20(7):870–5.
- Swain SS, Sharma D, Hussain T, Pati S.
Molecular mechanisms of underlying genetic
factors and associated mutations for drug
resistance in Mycobacterium tuberculosis.
Emerging Microbes and Infections.
2020;9(1):1651–63.
- Giri OP, Kumar A, Giri VP, Nikhil N. Impact of
Treatment Supporters on the Treatment Outcomes
of Drug Resistant-Tuberculosis (DR-TB) Patients:
A Retrospective Cohort Study. Cureus
[Internet]. 2022 Mar 6 [cited 2023 May
22]; Available from: https://www.cureus.com/articles/88412-impact-of-treatment-supporters-on-the-treatment-outcomes-of-drug-resistant-tuberculosis-dr-tb-patients-a-retrospective-cohort-study
- Aaina M, Venkatesh K, Usharani B, Anbazhagi M,
Rakesh G, Muthuraj M. Risk Factors and Treatment
Outcome Analysis Associated with Second-Line
Drug-Resistant Tuberculosis. Journal of
Respiration. 202128;2(1):1–12.
- Mannebach K, Dressel A, Eason L. Pediatric
tuberculosis in India: Justice and human rights.
Public Health Nursing.
2022;39(5):1058–64.
- Kiran B, Singla R, Singla N et al. Factors
affecting the treatment outcome of injection
based shorter MDR-TB regimen at a referral
centre in India. Monaldi Arch Chest Dis
[Internet]. 2022 Oct 5 [cited 2023 May 22]
- Prasad R, Singh A, Balasubramanian V, Gupta N.
Extensively drug-resistant tuberculosis in
India: Current evidence on diagnosis and
management. Indian J Med Res. 2017;145(3):271–93.
- Utpat K, Rajpurohit R, Desai U. Prevalence of
pre-extensively drug-resistant tuberculosis (Pre
XDR-TB) and extensively drug-resistant
tuberculosis (XDR-TB) among extra pulmonary (EP)
multidrug resistant tuberculosis (MDR-TB) at a
tertiary care center in Mumbai in pre
Bedaquiline (BDQ) era. Lung India.
2023;40(1):19.
- Laxmeshwar C, Das M, Mathur T, Israni T, Jha
S, Iyer A, et al. Psychiatric comorbidities
among patients with complex drug-resistant
tuberculosis in Mumbai, India. Dholakia YN,
editor. PLoS ONE. 2022;17(2):e0263759.
- India TB Report 2022 [Internet]. India:
Ministry of Health and Family Welfare Government
of India; 2022 [cited 2023 Jan 5] p. 263.
Available from: https://tbcindia.gov.in/WriteReadData/IndiaTBReport2022/TBAnnaulReport2022.pdf
- India TB Report 2019 [Internet]. India:
Ministry of Health and Family Welfare Government
of India; 2019 [cited 2023 Jan 5] p. 222.
Available from: https://tbcindia.gov.in/WriteReadData/India%20TB%20Report%202019.pdf
- India TB Report 2021 [Internet]. India:
Ministry of Health and Family Welfare Government
of India; 2021 [cited 2023 Jan 5] p. 329.
Available from: https://tbcindia.gov.in/showfile.php?lid=3587
- India TB Report 2020 [Internet]. India:
Ministry of Health and Family Welfare Government
of India; 2020 [cited 2023 Jan 5] p. 266.
Available from: https://tbcindia.gov.in/showfile.php?lid=3538
- Nair SA, Raizada N, Sachdeva KS, Denkinger C,
Schumacher S, Dewan P, et al. Factors Associated
with Tuberculosis and Rifampicin-Resistant
Tuberculosis amongst Symptomatic Patients in
India: A Retrospective Analysis. Subbian S,
editor. PLoS ONE. 2016 Feb
26;11(2):e0150054.
- Lohiya A, SuliankatchiAbdulkader R, Rath RS,
Jacob O, Chinnakali P, Goel AD, et al.
Prevalence and patterns of drug resistant
pulmonary tuberculosis in India—A systematic
review and meta-analysis. Journal of Global
Antimicrobial Resistance. 2020;22:308–16.
- Dzeyie KA, Basu S, Dikid T, Bhatnagar AK,
Chauhan LS, Narain JP. Epidemiological and
behavioural correlates of drug-resistant
tuberculosis in a Tertiary Care Centre, Delhi,
India. Indian Journal of Tuberculosis.
2019;66(3):331–6.
- Dorjee K, Sadutshang TD, Rana RS, Topgyal S,
Phunkyi D, Choetso T, et al. High prevalence of
rifampin-resistant tuberculosis in mountainous
districts of India. Indian Journal of
Tuberculosis. 2020;67(1):59–64.
- RivuBasu, Susmita Kundu, Debabani Biswas,
Saswati Nath, Sarkar A, Archita Bhattacharya.
Socio-Demographic and Clinical Profile of Drug
Resistant Tuberculosis Patients in a Tertiary
Care Centre of Kolkata. Indian J Community
Health. 2021;33(4):608–14.
- Ladha N, Bhardwaj P, Chauhan NK, Kh N, Nag VL,
Giribabu D. Determinants, risk factors and
spatial analysis of multi-drug resistant
pulmonary tuberculosis in Jodhpur, India. Monaldi
Arch Chest Dis [Internet]. 2022 Jan 18
[cited 2023 May 16]; Available from: https://monaldi-archives.org/index.php/macd/article/view/2026
- Nagarajan K, Kumarsamy K, Begum R, Panibatla
V, Reddy R, Adepu R, et al. A Dual Perspective
of Psycho-Social Barriers and Challenges
Experienced by Drug-Resistant TB Patients and
Their Caregivers through the Course of Diagnosis
and Treatment: Findings from a Qualitative Study
in Bengaluru and Hyderabad Districts of South
India. Antibiotics. 2022;11(11):1586.
- Sharma P, Lalwani J, Pandey P, Thakur A.
Factors associated with the development of
secondary multidrug-resistant tuberculosis. Int
J Prev Med. 2019;10(1):67.
- Husain AA, Kupz A, Kashyap RS. Controlling the
drug-resistant tuberculosis epidemic in India:
challenges and implications. Epidemiol
Health. 2021;43:e2021022.
- Ahmed S, Shukla I, Fatima N, Varshney S,
Shameem M, Tayyaba U. Profile of
drug-resistant-conferring mutations among new
and previously treated pulmonary tuberculosis
cases from Aligarh region of Northern India. Int
J Mycobacteriol. 2018;7(4):315.
- Srinivasan G, Chaturvedi D, Verma D, Pal H,
Khatoon H, Yadav D, et al. Prevalence of
depression and anxiety among drug resistant
tuberculosis: A study in North India. Indian
Journal of Tuberculosis. 2021;68(4):457–63.
- Kumar Sr, Shrinivasa B, Hissar Ss,
Rajasakthivel M. Ethical implications of the
National Tuberculosis Elimination Programme in
India: A framework-based analysis. Int J
Health Allied Sci. 2021;10(4):253.
- National Family Health Survey 2019-21
[Internet]. Government of India; 2021 [cited
2023 May 23]. Available from:
https://prsindia.org/policy/vital-stats/national-family-health-survey-5
- Mehta G, Sharma A, Arora SK. Human
Immunodeficiency Virus-1 Subtype-C Genetically
Diversify to Acquire Higher Replication
Competence in Human Host with Comorbidities. AIDS
Research and Human Retroviruses.
2021;37(5):391–8.
- Tegegne BS, Mengesha MM, Teferra AA, Awoke MA,
Habtewold TD. Association between diabetes
mellitus and multi-drug-resistant tuberculosis:
evidence from a systematic review and
meta-analysis. Syst Rev. 2018;7(1):161.
- Sachdeva KS, Parmar M, Patel Y, Gupta R,
Rathod S, Chauhan S, et al. Evolutionary journey
of programmatic services and treatment outcomes
among drug resistant tuberculosis (DR-TB)
patients under National TB Elimination Programme
in India (2005-2020). Expert Review of
Respiratory Medicine. 2021;15(7):885–98.
|



















