|
Introduction:
Metastatic
deposits to the breast from extramammary
malignancies are rare and account for only 0.3% to
2.7% of all malignant breast tumors [1,2]. Clinically
and radiologically, metastatic malignancies from
extramammary sites may masquerade neoplasms of the
breast, sometimes even benign ones [1]. A correct
diagnosis of metastasis to the breast is of
paramount importance as the treatment of primary
and secondary malignancies of the breast is
different.
We have reviewed 4
cases of metastatic neoplasms to the breast which
were diagnosed in the 5-year period. Metastases
from primary breast carcinoma were excluded.
Case Reports
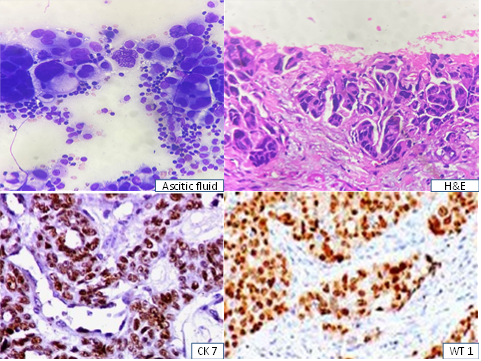
Case 1:
A 67-year-old
postmenopausal lady was on chemotherapy and
regular follow-up as biopsy from her neck nodes
revealed metastatic deposits of unknown origin. 19
months later, she came with complaints of
abdominal pain. On examination, she was found to
have ascites. USG abdomen revealed moderate
ascites with right ovarian cyst and septations.
Omental nodule was also seen. The ascitic fluid
was aspirated and USG-guided FNAC of the omental
nodule was done. Both the samples revealed
pleomorphic cells arranged in clusters and
papillaroid patterns with signet ring cells
(Figure 1a). Immunohistochemical analysis on the
cell block, showed tumor cells positive for CK7
and WT1 (Figure 1b). She was diagnosed with
metastatic adenocarcinomatous deposits from ovary.
10 months later, the patient came with lump in
both breasts. She had noticed the lump first in
the right breast and then in the left. USG-guided
trucut biopsy was performed and it revealed
malignant cells with the same morphology as that
described in the omental nodule.
Immunohistochemistry was done and the neoplastic
cells expressed strong positivity with WT1 and
PAX8. They were negative for GCDFP-15 (Figure 1c),
thus ruling out a primary breast carcinoma.
|
| Fig.1
- Ovarian serous papillary adenocarcinoma
|
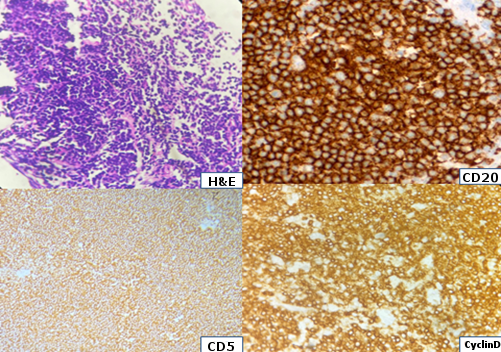
Case 2:
A 43-year-old lady,
presented with lump in the left breast. Clinically
and radiologically, it was diagnosed as carcinoma
breast. USG-guided trucut biopsy was done and it
showed monotonous population of small round blue
cells arranged in diffuse sheets (Figure 2). After
further immunohistochemical markers study, it was
diagnosed as mantle cell lymphoma. On further
detailing, it was revealed that 6 months earlier,
patient had generalised lymphadenopathy and biopsy
of the cervical lymph node was done. On retrieving
the cervical lymph node biopsy sections, it showed
monotonous population of small round cells with
the same morphology as that seen in breast, and
the immunohistochemistry confirmed it to be non
Hodgkin lymphoma (Mantle cell type). The breast
diagnosis was given as metastatic lymphoma. She is
currently on chemotherapy.
|
| Fig.2
– NHL - Mantle cell lymphoma |
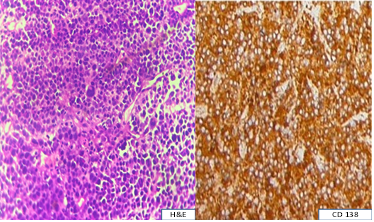
Case 3:
A 37-year-old lady
presented with complaints of abdominal distension,
pain abdomen and decreased urine output. On
physical examination, there was ascites and
bilateral hard breast lumps. The patient
attributed the hard lumps in the breasts to her
sudden weaning from breastfeeding her 1 and half
year baby, due to her general weakness. Her CT
abdomen revealed pancreatitis, superior mesenteric
vein thrombosis and a pancreatic lesion with lytic
lesions in the pelvic bone. Findings were
initially suggestive of primary lesion in the
pancreas or bilateral breasts which would have
given rise to several bony secondaries. Ascitic
fluid analysis showed florid mesothelial cell
hyperplasia with scattered atypical cells. Trucut
biopsy from the breast revealed a poorly
differentiated neoplasm (Figure 3a) which was
diagnosed as plasmacytoma after IHC studies
(Figure 3b). Her creatinine was elevated and she
had to be put on dialysis. Serum protein
electrophoresis done on the consecutive days,
revealed monoclonal spike in the gamma region.
Bone marrow aspiration and biopsy were done and it
was diagnosed as plasma cell dyscrasia (Figure
3c). Surgery for the breast lumps was diverted and
patient was started on chemotherapy for Multiple
Myeloma.
|
| Fig.3
- Plasmacytoma |
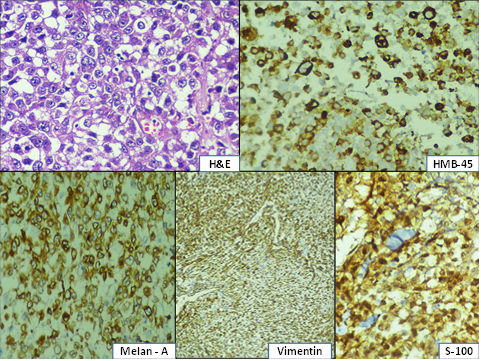
Case 4:
A 54-year-old
postmenopausal lady presented with complaints of
swelling in the right inguinal region since 4
months and lump in the left breast since 2 months.
She gave past history of foot ulcer excision which
was diagnosed as malignant melanoma, 2 years ago.
USG-guided trucut biopsy of the breast lump was
done at another center and was reported as
invasive ductal carcinoma. At our center, PET scan
was done which showed uptakes in the right
inguinal region and breast with no uptake
elsewhere. Based on the reports, a provisional
diagnosis of double malignancy (left breast
carcinoma and right inguinal malignant melanoma)
was made. She underwent left modified radical
mastectomy and right ileo-inguinal block
dissection. The biopsy sections of the mastectomy
specimen and inguinal nodes revealed same
morphology of sheets of pleomorphic cells arranged
in sheets with intracytoplasmic and extracellular
pigment deposition (Figure 4a). The diagnosis on
the mastectomy specimen was given as metastatic
malignant melanoma after IHC studies (Figure 4b).
She is currently on chemotherapy.
|
| Fig.4
– Malignant melanoma |
Hence from the above
discussed cases, 2 cases presented with breast
lump during presentation, of which 1 was
misdiagnosed as primary breast carcinoma. Had it
been diagnosed as secondaries in breast, treatment
would have been restricted to palliative
chemotherapy and a modified radical mastectomy
could have been avoided. This highlights the
significance of relevant clinical history, correct
histopathological diagnosis and the challenge
behind differentiating secondaries in breast from
primary breast disease.
Discussion
Secondaries to the
breast are rare. In large studies they have been
reported to constitute 0.3–2.7% of all breast
malignancies [1-3]. The most common are lymphomas,
tumors of hematopoietic origin, followed by
ovarian adenocarcinoma, malignant melanoma and
bronchogenic carcinomas [4,5]. Clinically, a
breast metastasis usually presents as a rapidly
growing, single, firm mass that is usually mobile,
not tender and located more often in the left
breast and the upper outer quadrant. Both breasts
can be involved. Typically, tumours appear
discretely in the breast displacing normal breast
tissue rather than arising from them [6]. By
imaging, many different appearances of metastatic
tumors in the breast can be seen. They may
masquerade as a probably benign lesion or could be
similar to primary breast carcinomas [7, 8]. Lee
et al reported that only 2 cases in their series
of 33 cases, were classified as BIRADS 3, the rest
being categorized as BIRADS 4b or higher [8].
The majority of
patients who present clinically with metastatic
breast tumour have a known primary elsewhere.
However, a small subset of patients present with
occult primary disease and breast metastases are
the first manifestation of the disease. Metastatic
melanoma is a mimicker of a broad spectrum of
primary breast lesions. Due to the varied
morphological patterns, including epithelioid,
spindle and plasmacytoid cells, there could be
overlap with mammary carcinoma. Awareness of this
is essential to avoid inappropriate treatment,
especially in ‘‘triple negative,’’ poorly
differentiated carcinomas of the breast. Although
the application of a simple panel of antibodies
assists in correct interpretation, lesions
presenting as isolated breast tumors may introduce
a significant diagnostic difficulty, especially
when there is inadequate patient history and
limited biopsy material. A long interval between
primary diagnosis or the first appearance of
malignancy and breast metastases could also result
in misdiagnosis of the tumour for an infiltrating
primary carcinoma of breast. Therefore, along with
biopsy sections, a good clinical history and
application of immunohistochemical stains is
mandatory.
Treatment of breast
metastases should be directed at the primary
disease. Surgical therapy is widely recommended to
be mostly conservative whenever possible and
commonly entails wide local excision. Treatment
for isolated metastatic disease may be palliated
by surgical resection with few cases having good
prognosis. In the majority of cases the prognosis
is poor. Large bulky tumours may be palliated by
mastectomy though this procedure should be avoided
whenever possible. In specific tumours such as
carcinoid, lymphomas and choriocarcinomas,
chemotherapy is found to give symptomatic relief
with prolonged survival in select patients.
Survival in patients with metastatic lymphoma is
related to stage and histologic characteristics.
Patients with higher grade histologic lesions or
more advanced stage have a worse prognosis.
Advanced melanoma, though usually refractory to
systemic therapy, may occasionally respond to
treatment with biologic response modifiers and
cytotoxic agents.
Conclusion
Metastases to the
breast needs to be considered if the histological
appearance is unusual for a primary mammary
tumour. In some cases the histological appearance
is similar to a primary mammary tumour and hence
the clinical history with relevant investigations
are essential to making the accurate diagnosis and
definite management.
References
- Buisman FE, van Gelder L, Menke-Pluijmers MB,
Bisschops BH, Plaisier PW, Westenend PJ.
Non-primary breast malignancies: a single
institution's experience of a diagnostic
challenge with important therapeutic
consequences-a retrospective study. World J
Surg Oncol. 2016 Jun 23;14(1):166. doi:
10.1186/s12957-016-0915-4.
- Lee SK, Kim WW, Kim SH, et al. Characteristics
of metastasis in the breast from extramammary
malignancies. J Surg Oncol. 2010;101
(2):137–140. doi:10.1002/jso.214534
- Güldoğan N, Esen İçten G, Tokat F, Tutar B,
Kara H, Korkmaz T, Oyan Uluç B, Demir G. Three
Cases of Breast Metastases from Lung Cancer and
Systematic Review of the Literature. Eur J
Breast Health 2021; 17(2): 200-205.
- Mun SH, Ko EY, Han BK, Shin JH, Kim SJ, Cho
EY. Breast metastases from extramammary
malignancies: typical and atypical ultrasound
features. Korean J Radiol 2014; 15:
20-28.
- Ota T, Hasegawa Y, Okimura A, Sakashita K,
Sunami T, Yukimoto K, et al. Breast metastasis
from EGFR-mutated lung adenocarcinoma: A case
report and review of the literature. Clin
Case Rep 2018; 6: 1510-1516.
- Williams SA, Ehlers RA 2nd, Hunt KK, Yi M,
Kuerer HM, Singletary SE, et al. Metastases to
the breast from nonbreast solid neoplasms:
presentation and determinants of survival. Cancer
2007; 110: 731-737.
- Bitencourt AGV, Gama RRM, Graziano L, Negrão
EMS, Sabino SMPS, Watanabe AHU, et al. Breast
metastases from extramammary malignancies:
multimodality imaging aspects. Br J Radiol 2017;
90: 2017-2197. (PMID: 28485985)
- Lee JH, Kim SH, Kang BJ, Cha ES, Kim HS, Choi
JJ. Metastases to the breast from extramammary
malignancies - sonographic features. J Clin
Ultrasound 2011; 39: 248-255.
|



















