|
Introduction:
Air
pollution is caused by the contamination of indoor
or outdoor environments by chemical, physical, or
biological agents. The World Health Organization
(WHO) reports particulate matter (PM), carbon
monoxide (CO), ozone (O3), nitrogen
dioxide (NO2), and sulphur dioxide (SO2)
as pollutants of major public health concern.(1)
Both outdoor or ambient and household air
pollution (HAP), also known as indoor air
pollution (IAP), pose serious health risks.(2)
Statistics suggest that the health impacts of HAP
far outweigh those of outdoor air pollution,
especially in developing countries. HAP can be up
to ten times worse than outdoor air pollution
because enclosed spaces allow pollutants to
accumulate more than open spaces.(3) HAP is
estimated to risk the health of around 2.6 billion
people who do not have access to clean cooking
fuel and who are still dependent on biomass or
solid fuels for cooking.(4) Around 3.8 million
premature deaths were attributable to HAP in 2016,
among these deaths, 27% were due to pneumonia, 18%
from stroke, 27% from ischemic heart disease
(IHD), 20% from chronic obstructive pulmonary
disease (COPD) and 8% from lung cancer. (5)
The principal
sources of HAP are the combustion of fuels or
other items; however, incomplete combustion of
biomass is the main source of HAP worldwide. (6)
Inefficient combustion of solid fuels results in
products of incomplete combustion, including
particles, gases, and a multitude of compounds
that are known toxicants. (7) Exposure to such
toxic pollutants and PM increases the risk of
developing several diseases that have been majorly
categorised into categories such as
cardiovascular, neurological, respiratory, and
cancer. (8)
PM emitted by common
solid fuels, in particular, is of concern due to
its ability to cross the alveolar membrane and
enter the circulation, where it can interact
directly with the vascular endothelium and cardiac
cells, ultimately leading to cardiovascular
diseases. (9)
High BP or
hypertension (HTN) is one of the leading global
risk factors for cardiovascular diseases,
affecting more than one billion individuals and
causing 9.4 million deaths each year. (10) Every
20 mmHg increase in systolic blood pressure (SBP)
or 10 mmHg increase in diastolic blood pressure
(DBP) above 115/75 mmHg has been shown to be
associated with more than a two-fold increase in
cardiovascular mortality. (11) Because PM2.5 and
high BP are both independently leading risk
factors for premature death around the world,
several researchers have investigated the
potential link between these two factors.
In 2008, Fullerton
and colleagues published a non-systematic review
of research on the health effects of HAP from
biomass fuel, including cardiovascular disease,
and found a scarcity of relevant data. (12) In
another review article published in 2016, only a
section of the paper discusses the relationship
between IAP exposure and BP. (13) A systematic
review by Zafar and David assessed the strength of
the evidence for an association of coronary heart
disease with HAP from solid fuel use and the
likely magnitude of any increase in risk. (14)
However, over the last few years, research
studying associations between HAP from solid fuel
burning and HTN risk has been expanding; we,
therefore, undertook a narrative evaluation of
systematically identified articles with the aim to
summarise recent evidence linking HAP due to
biomass fuel and BP or HTN among human
participants.
Methods:
Data Sources
and Search Strategies: We searched
three electronic databases (PubMed, CORE, and
Semantic Scholar) for articles published starting
from the inception of these databases to March 31,
2022. The search strategy included keywords
related to blood pressure and HAP or biomass. In
addition, we reviewed the full text of relevant
cross-references from each search result.
Article selection: Inclusion and
exclusion criteria
Type of study: All
randomized controlled trials (RCTs and
quasi-RCTs), non-randomized control trials (that
is, cohort, case-controlled, and cross-sectional
studies), and controlled before-and-after studies
were included.
Types of articles:
We considered articles published in peer-reviewed
journals. Studies or articles that are general and
only report HAP, fuel use, and non-indoor or
ambient air quality/health-related outcomes were
excluded.
After conducting a
search on the mentioned databases, all articles
were imported into EndNote software (Thomson
Reuters 2009) to remove duplicates. After that, a
title and abstract screening were conducted, and
on the basis of inclusion/exclusion criteria,
ineligible articles were excluded. A detailed
review of the remaining articles was carried out,
and if any of them did not fulfill the
inclusion/exclusion criteria, they were further
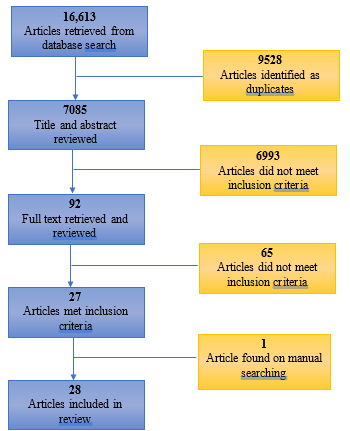
excluded. Figure 1 depicts a chart for this
process.
|
| Figure
1: Flow diagram for study
selection |
Overall, of the
total articles obtained through searches in the
databases and manual tracking, 28 articles formed
part of this review article.
To ensure the
unbiased selection and correct identification of
articles, two independent investigators conducted
an initial screening and examined the full text of
each potentially relevant article. If there was
any contradiction, it was resolved through
discussion among all the authors.
Data
extraction: The following information
was extracted from all of the included articles:
author name, publication year, title of the paper,
journal information, geographic location, type of
study, study population, sample size and age, sex
proportion, fuel type, short-term or long-term
effect assessment, type of air pollutant measured,
BP measurements, and confounding factors. The
information extracted from all of the included
articles is detailed in Table 1.
|
Table 1: Characteristics of the
included articles
|
|
Author/Year
|
Short/Long term
|
Location
|
Participants
|
Sample Size
|
Air Pollutant Measured
|
Outcome
|
Addressed confounders
|
|
Mohapatra I, et al., 2018 (15)
|
Long
|
India
|
Women
Age: 20-40 years
|
193
|
NA
|
Hypertension was found to be associated
with number of cooking years and was also
found to be statistically significant (P =
0.0065)
|
-
|
|
Young B, et al., 2019 (16)
|
Short
|
Rural Honduras
|
Women
Age: 25-56 years
|
147
Traditional stove: 74
Intervention stove: 73
|
PM2.5
Black Carbon
|
Elevated SBP and DBP were associated with
exposure to HAP from biomass cookstoves
compared to intervention cookstoves
Kitchen v. Personal PM2.5: The
associations between kitchen PM2.5
and BP were stronger than those for
personal PM2.5
|
Age
BMI
|
|
Ofori S, et al., 2018 (17)
|
Short
|
South Nigeria
|
Women
Age: ≥18 years
|
389
|
PM2.5
|
The use of biomass fuel use was
significantly associated with 2.7 mmHg
higher SBP (p ¼ 0.040), in addition to
increased odds of pre-hypertension (OR
1.67 95% CI 1.56, 4.99, P ¼ 0.035) but not
hypertension (OR 1.23 95% CI 0.73, 2.07, P
¼ 0.440).
|
Cigarette smoker, exposed to passive
smoke in household,
consumes alcohol, history of hypertension,
history of diabetes, Total cholesterol
|
|
Arku et al., 2018 (18)
|
Long
|
Albania, Armenia,
Azerbaijan, Bangladesh, Benin, Ghana,
Kyrgyzstan, Lesotho, Namibia, and Peru
|
Premenopausal women Age: 15–49 years
|
77,605
|
NA
|
In adjusted, pooled analyses, primary use
of solid fuel was associated with 0.58
mmHg higher SBP (95% CI: 0.23, 0.93) as
compared to use of clean fuel.
The pooled estimates for DBP were
positive, but the confidence intervals
contained zero.
Solid fuel use was associated with 16%
greater odds of hypertension [OR = 1.16
(95% CI: 1.01, 1.35)].
|
Age, BMI, ethnicity, education,
occupation, wealth index, rural/urban
location, and month of interview in
country
|
|
Neupane M et al., 2015 (19)
|
Long
|
Nepal
|
Women
Age: ≥ 30 years
|
Biogas: 219
Firewood: 300
|
CO
|
Participant aged >50 years: Use of
biogas was associated with 9.8 mmHg lower
SBP and 6.5 mmHg lower DBP compared to
firewood users. In this age group, biogas
use was also associated with 68% reduced
odds of developing hypertension.
These effects were not identified in
younger women aged 30–50 years.
|
Smoking, kitchen characteristics,
ventilation status and
additional fuel use
|
|
Lee et al., 2012 (20)
|
Long
|
China
|
Mixed
Age: ≥18 years
|
13,438
|
NA
|
The use of solid fuel in home was
significantly associated with an increased
risk for hypertension after adjusting for
potential confounders.
|
Age, gender, education, second-hand
smoke, and smoking status
|
|
Yan Z et al., 2016 (21)
|
Long
|
China
|
Mixed
Age: ≥18 years
|
4,594
|
NA
|
After adjusting for potential
confounders, 0.75% higher SBP and 1.05%
higher DBP and increased risk for
hypertension in current solid fuel users
was observed.
Users with longest duration of solid fuel
exposure had a 1.63% higher SBP, 1.31%
higher DBP and larger risk of hypertension
with an OR of 1.55 than non-users.
|
Age, age squares, gender, region (rural,
urban), education,
household income (low, medium, high), BMI,
WC, diet habit (daily salt, fat, protein
intake), smoking status, alcohol intake,
physical activity level (light, moderate,
heavy)
|
|
Pena MB et al., 2015 (22)
|
Long
|
Peru
|
Mixed
Age: ≥35 years
|
1,004
|
NA
|
Association between biomass fuel use with
both prehypertension and hypertension was
observed.
Biomass fuel users had a higher SBP and
DBP when compared with nonusers.
Interaction between daily biomass fuel use
and sex or percent predicted forced vital
capacity for either SBP or DBP was not
observed.
|
Sex, age, body mass index, height,
wealth, education years,
depressive symptoms, smoking, alcohol
abuse and low physical activity
|
|
Fatmi Z et al., 2016 (14)
|
Long
|
Pakistan
|
Women
Age: ≥40 years
|
Biomass:436
Non-biomass: 414
|
NA
|
After adjustment for potential
confounders, there was no association of
hypertension with current use of biomass
for cooking.
Nor were any associations apparent when
analyses were restricted to long-term (≥10
years) users and non-users of biomass
fuel.
|
Birth weight, Smoking, Weight,
Consumption of meat or eggs
BMI, Nutrition
|
|
Baumgartner J et al., 2011 (23)
|
Short
|
China
|
Women
Age: ≥ 25 years
|
280
|
PM2.5
|
A 1-log-µg/m3 increase in PM2.5
exposure was associated with 2.2 mmHg
higher SBP and 0.5 mmHg higher DBP.
Women > 50 years of age: A 1-log-µg/m3
increase in PM2.5 exposure was
associated with 4.1 mmHg higher SBP and
1.8 mmHg higher DBP.
Younger women: PM2.5 exposure
was positively associated with SBP but the
association was not statistically
significant
|
Season, Age, Obesity, Physical activity,
Salt intake
|
|
McCracken JP et al., 2007 (24)
|
Short
|
Guatemala
|
Women
Age: >38 years
|
Intervention group: 49
Control group: 71
|
PM2.5
|
After adjusting for potential
confounders, the improved stove
intervention was associated with 3.7 mmHg
lower SBP and 3.0 mmHg lower DBP (95% CI,
–5.7 to –0.4) compared with controls.
|
Age, body mass index, an asset index,
smoking, second hand tobacco smoke,
apparent temperature, season, day of week,
time of day, and a random subject
intercept
|
|
Clark ML et al., 2011 (25)
|
Short
|
Nicaragua
|
Women
Age: 11-80 years
|
123
|
PM2.5
CO
|
There was weak but suggestive evidence of
associations of PM2.5 and CO
with indicators of cardiovascular health
(blood pressure and heart rate), some of
which were stronger among obese women than
non-obese women.
|
-
|
|
Aung TW, et al., 2018 (26)
|
Short
|
India
|
Women
Age: >25 years
|
Intervention: 92
Control:46
|
PM2.5
Black Carbon
|
Lower SBP and DBP was observed among
exclusive users of intervention stove,
although confidence intervals included
zero.
Stacking or mixed use of intervention and
traditional stoves contributed to a small
increase in SBP and DBP.
Median air pollutant concentrations
increased post-intervention in all stove
groups, with the lowest median PM2.5
increase in the exclusive intervention
stove group.
|
Age, BMI
|
|
Norris C, et al., 2016 (27)
|
Short
|
India
|
Women
Age: 25-66 years
|
45
|
Black carbon
|
Interquartile range increases in black
carbon were associated with changes in SBP
and small decrease in DBP
|
Age, temperature, BMI, SES, salt intake,
time of day, and physical activity
|
|
Chakraborty D and Mondal N, 2018 (28)
|
Long
|
India
|
Women
Age: 22-62 years
|
Biomass: 60
LPG: 32
|
CO, CO2, O3, SO2,
TSPM, PM2.5, PM10
|
Age: The association between use of
household fuel and SBP was stronger among
the group with age above 50 compared with
subjects under 50 years old
Pollutants: The kitchen room pollutant
concentrations in the case of biomass
users were positively linked with SBP, DBP
|
-
|
|
Wylie B, et al., 2015 (29)
|
Not given
|
India
|
Pregnant Women
|
Wood: 1134 Gas:
235
|
NA
|
In pregnant women, compared to gas users,
women using wood as fuel had on average
lower mean arterial pressure and DBP at
delivery. Risk of hypertension (systolic
> 139 mmHg or diastolic > 89 mmHg)
was 14.6% for women cooking with wood
compared to 19.6% for those cooking with
gas although this did not reach
significance after adjustment, using
propensity score techniques, for factors
that make wood and gas users distinct
|
Cohort (Jharkhand versus Chhattisgarh),
history of hypertension, presence of
windows, and use of smokeless tobacco
|
|
Dutta A et al., 2011(30)
|
Long
|
India
|
Premenopausal Women
Age: >15 years
|
Biomass: 244
LPG: 236
|
PM10
PM2.5
|
After controlling potential confounders,
hypertension was positively associated
with both PM10 and PM2.5
Compared with those having 5–14 years
cooking experience (25.4%), hypertension
was more prevalent in women cooking for 15
years or more (34.2%) with biomass, but
the difference was not significant in
Chi-square test (P = 0.08).
|
Sex, Smoking
|
|
Dutta A et al., 2012(31)
|
Long
|
India
|
Women
|
Biomass: 635
LPG: 452
|
PM10
PM2.5
|
Compared with control, biomass users had
more particulate pollution in indoor air.
PM10 and PM2.5
levels were positively associated with
hypertension.
|
Age, BMI, years of cooking and family
income
|
|
Ray MR et al., 2006 (32)
|
Long
|
India
|
Women
|
LPG: 155
Biomass:165
|
PM10
PM2.5
|
Prevalence of hypertension was found to
be 3.2% in LPG users and 6.0% in biomass
users
|
Age, smoking, tobacco chewing and
environmental tobacco smoke
|
|
Chakraborty D, 2014 (6)
|
Short
|
India
|
Women
|
50
|
CO, CO2 and O3
|
Age: Both SBP and DBP showed a strong
positive (p < 0.05) relationship with
age of biomass users.
Wood users suffer from high SBP (p <
0.037)
|
-
|
|
Dutta and Ray, 2013 (33)
|
Long
|
India
|
Premenopausal Women
|
Biomass: 244
LPG: 236
|
PM10
PM2.5
|
Significant positive association between
exposure variables and hypertension were
noticed, after adjusting for potential
confounders
|
Age, exposure years, kitchen location,
family income, and education
|
|
Arku et al., 2020 (34)
|
Long
|
India
|
Mixed
|
43,313
|
NA
|
Non-linear patterns were observed for SBP
and DBP.
Individuals who used solid fuels for
cooking had lower BP measures compared to
clean fuel users (e.g. 34% of solid fuels
users compared to 42% of clean fuel users
had hypertension), and even in fully
adjusted models had slightly decreased
odds of hypertension (OR ¼ 0.93; 95% CI:
0.88, 0.99) and reductions in SBP (0.51
mmHg; 95% CI: 0.99, 0.03) and DBP ( 0.46
mmHg; 95% CI: 0.75, 0.18).
In this large international multi-center
study, chronic exposures to outdoor PM2.5
was associated with increased BP and
hypertension while there were small
inverse associations with HAP.
|
Age, Smokers, Alcohol users
|
|
Barman, et al., 2019 (35)
|
Long
|
Bangladesh
|
Women
Age: 19–60 years
|
410
|
NA
|
Participants age ≥40 years: Cumulative
exposure to biomass smoke were found to be
the significant risk factors of
hypertension.
Every 1 year increase in cumulative
exposure to biomass smoke eventually
exacerbated the risk of hypertension by
61% (adjusted odds ratio 1.61, 95%
confidence interval: 1.16–2.22; P <
0.01).
|
Age, history of smokeless tobacco,
parental history of
hypertension, and BMI
|
|
Abba et al., 2016 (36)
|
NA
|
Albania
|
Mixed
Age: ≥15 years
|
20,846
|
NA
|
Participants exposed to household
polluting fuels were 17% more likely to
develop hypertension than those not
exposed to household air pollution
Odds of hypertension were more significant
among women, rural residents and
participants aged >24 years who were
exposed to household polluting fuels
compared to their counterparts who were
not exposed.
|
-
|
|
Quinn et al., 2017 (37)
|
NA
|
Ghana
|
Women
Age: 23-29 years
|
44
|
CO
|
Peak CO exposure (defined as ≥4.1 ppm) in
the 2 hours prior to BP measurement was
associated with elevations in hourly SBP
and DBP as compared to BP following lower
CO exposures.
Women receiving improved cookstoves had
lower post-intervention SBP, though this
result did not reach statistical
significance.
|
Gestational age and type of BP assessment
(ABPM vs. HPBM)
|
|
Clark et al., 2019 (38)
|
Long
|
China
|
Women
Mean age: 52.3 years
|
205
|
PM2.5
|
Women who did not receive the energy
package had greater mean decreases in
brachial SBP and DBP compared with women
who received the package. Similar trends
were found for central BP.
No evidence was found that distribution of
a high-performing, multi-purpose
semi-gasifier stove and supply of
processed biomass fuel resulted in
improvements in BP, after one and a half
years of follow-up.
|
Age (years), ethnicity (Han or Qiang),
socioeconomic status, body mass index
(BMI, kg/m2), current use of hypertension
medication (yes/no), presence of a tobacco
smoker in the home (yes/no), daily sodium
intake (g/day), physical activity
(steps/day), outdoor and indoor
temperature (Celsius degrees), season
(summer versus winter), and household
location
|
|
Alexander et al., 2014 (39)
|
Long
|
Bolivia
|
Women
Age: 23-81 years
|
28
|
PM
|
Mean SBP decreased after the improved
cookstove intervention.
Small decreases in DBP were also seen, but
these changes were not significant.
Stronger correlations were found between
reductions in cooking PM concentrations
and reductions in both SBP and DBP.
|
-
|
|
Alexander et al., 2017 (40)
|
NA
|
Nigeria
|
Pregnant
women
|
324
|
NA
|
The change in DBP over time was
significantly different between ethanol
users and control subjects however SBP did
not differ.
Mean DBP was 2.8 mmHg higher in control
subjects than in ethanol users and 6.4% of
control subjects were hypertensive (SBP
>140 and/or DBP >90 mmHg) versus
1.9% of ethanol users (P = 0.051).
Among pre-intervention kerosene users,
8.8% of control subjects were hypertensive
compared with 1.8% of ethanol users.
|
-
|
|
BMI – Body Mass Index, CI – Confidence
Interval, CO – Carbon monoxide, CO2 –
Carbon dioxide, DBP – Diastolic blood
pressure, HAP – Household air pollution,
LPG – Liquefied Petroleum Gas, O3 –
Ozone, PM – Particulate matter, SBP –
Systolic blood pressure, TSPM - Total
Suspended Particulate Matter
|
Results
Search
results and characteristics of the included
studies: As shown in Figure 1, 16,613
articles were identified through a systematically
crafted search strategy. After removing duplicate
articles and considering the inclusion/exclusion
criteria, 92 articles were examined. Among these
92 articles, 65 were excluded after examining the
full text because of insufficient data, repeated
studies, or research not relevant for inclusion in
the current review article. Twenty-eight (28)
articles were finally included in this review.
Table 1 depicts the summarized data from the 28
included articles.
Pollutants
released from solid fuel: Solid fuel
combustion produces a large number of
health-damaging air pollutants, such as respirable
PM, nitrogen oxides, carbon monoxide (CO),
formaldehyde, 1,3 butadiene, benzene, polycyclic
aromatic hydrocarbons, and many other toxic
organic compounds. (15)
Seventeen of the 28
articles have measured the levels of various
pollutants emitted by different fuels, including
PM, CO, and black carbon (BC).
The majority of the
studies (13 out of 28) have measured levels of PM,
predominantly PM10 and PM2.5.
The concentrations of PM and time points tested
are variable across the studies. The two most
commonly used dose metrics are μg/cm2
or μg/ml. A summarised version of PM measurement
is depicted in Table 2.
|
Table 2: Particulate matter
measurement across different studies
|
|
Author/Year
|
Type of PM
|
Duration
|
PM measurements
|
|
Young B,
et al. 2019
(16)
|
PM2.5
|
24-hour average
|
CASE
Personal (n=104): 126 μg/m3
Kitchen (n=105): 360 μg/m3
|
CONTROL
Personal (n=104): 66 μg/m3
Kitchen (n=105): 137 μg/m3
|
|
Ofori S, et
al. 2018
(17)
|
PM2.5
|
Six times a day
|
BIOMASS
Cook time v. non-cook time: 196.3 ± 24.5
v. 12.3 ± 5.7 mg/m3
|
NON-BIOMASS
Cook time v. non-cook time:
non-BMF: 79.5 ± 13.3 v. 4.6 ± 0.6 mg/m3
|
|
Baumgart
ner J et al.
2011
(23)
|
PM2.5
|
24-hour exposure
|
SUMMER (n=18)
Personal: 9 to 492 µg/m3
Geometric mean: 55 µg/m3
|
WINTER (n=66)
Personal: 22 to 634 µg/m3
Geometric mean: 117 µg/m3
|
|
McCracke
n JP et al.
2007
(24)
|
PM2.5
|
24-hour
|
CASE (n=49): 264 µg/m3
|
CONTROL (n=71): 102 µg/m3
|
|
Clark ML
et al. 2011
(25)
|
PM2.5
|
48-hour
|
n=115; 154–6,901 µg/m3
Mean: 1354 µg/m3
|
|
Aung TW,
et al. 2018
(26)
|
PM2.5
|
Median air pollutant concentrations
increased post-intervention in all stove
groups, with the lowest median PM2.5
increase in the exclusive intervention
stove group
*Values not available
|
|
Chakraborty D and Mondal N
2018
(28)
|
PM2.5, PM10
|
24-hour
|
The concentrations of all the pollutants
were significantly (p < 0.001) higher
in biomass users than in LPG-using
households
*Values not available
|
|
Dutta A,
et al. 2011
(30),
Dutta A,
et al. 2012
(31),
Dutta and
Ray 2013
(33)
|
PM10
|
8-hour mean concentration
|
CASE (n = 244)
276 ± 108 (SD) μg/m3
|
CONTROL (n = 236)
97 ± 36 μg/m3
|
|
PM2.5
|
CASE (n = 244)
156 ± 63 (SD) μg/m3
|
CONTROL (n = 236)
52 ± 27 μg/m3
|
|
Ray MR
et al. 2006
(32)
|
PM10
|
Cooking and non-cooking hours (mean)
|
CASE (n = 165)
Cooking: 625 μg/m3
Non-cooking: 204 μg/m3
|
CONTROL (n = 155)
Cooking: 169 μg/m3
Non-cooking: 93 μg/m3
|
|
PM2.5
|
CASE (n = 165)
Cooking: 312 μg/m3
Non-cooking: 108 μg/m3
|
CONTROL (n = 155)
Cooking: 77 μg/m3
Non-cooking: 45 μg/m3
|
|
Clark et
al. 2019
(38)
|
PM2.5
|
48-hour
|
SUMMER (n = 204)
Without energy pack
Pre v. Post Intervention: 90.7 v. 47.3
μg/m3
With energy pack
Pre v. Post Intervention: 74.1 v. 51.5
μg/m3
|
WINTER (n = 204)
Without energy pack
Pre v. Post Intervention: 201.3 v. 205.1
μg/m3
With energy pack
Pre v. Post Intervention: 153.3 v. 107.0
μg/m3
|
|
Alexander
et al. 2014
(39)
|
PM
|
24-hour
(mean)
|
PRE-INTERVENTION (n = 15)
Kitchen: 240 μg/m3 ±210
Personal: 780 μg/m3 ±440
|
POST-INTERVENTION (n = 15)
Kitchen: 48 μg/m3±41
Personal: 135 μg/m3 ± 97
|
|
PM – Particulate matter
|
Associations
between PM and other pollutants exposure and BP:
Majority of the research studies included
in this review article linking BP or HTN with
emissions from solid fuel use focus on PM.
The study done by
Young B et al. in rural Honduras showed that
traditional stoves produced substantially higher
24-hour mean personal and kitchen PM2.5 and
BC concentrations compared to interventional
stoves. The study results provide evidence that
one unit increase in kitchen PM2.5
concentration was associated with 2.5 mmHg higher
SBP. However, the associations between kitchen PM2.5
concentrations and BP were stronger than those for
personal PM2.5, which is contradictory
to the general consensus. (16)
These findings are
consistent with a randomized intervention study
among Guatemalan women, which observed that daily
average PM2.5 exposures were 264 and
102 µg/m3 in the control and
intervention groups, respectively. Compared with
controls, the intervention group had 3.7 mmHg
lower SBP and 3.0 mmHg lower DBP. (24)
Studies by Dutta et
al. provide consistent evidence that biomass users
who had three times more PM pollution in the
kitchen had a higher prevalence of HTN compared to
non-biomass users, suggesting a positive
association between HAP and increased
cardiovascular risk.(30, 31, 33)
Among other
components of particulate pollution, several
research studies (16,26, 27) have reported higher
BP after exposure to BC.
Yet another
pollutant which was majorly studied by most
researchers was CO. Clark et al. examined the
cardiovascular effects of indoor and personal CO
concentrations in Nicaragua. They found
nonsignificant elevations in SBP due to an
increase in 48-hour indoor CO (1.78 mmHg increase
in SBP per 24 ppm). Although statistically
nonsignificant it is still suggestive of an
increase. (25)
Associations
between long term exposure to HAP and BP: Multiple
studies have shown that long-term exposure (>1
year) to HAP from biomass has positive
associations with BP. Table 1 provides a
comprehensive summary of the results regarding the
long-term impacts of HAP exposures on BP.
Among the numerous
articles reported in Table 1, a few of the most
notable articles that best exemplify the majority
of findings have been chosen for further
discussion. In a cross-sectional study conducted
by Mohapatra et al. in the Odisha region of India,
HTN was found to be associated with the number of
cooking years and was also found to be
statistically significant in women who regularly
cooked with biomass for ≥ 5 years. (15)
Lee et al. showed a
significant association between HTN and biomass
fuel smoke in China, who had, on average, 19 years
of household solid fuel exposure. (20)
A cross-sectional
study by Dutta et al. 2011 also indicated that
apparently healthy, pre-menopausal, married,
non-smoking, tobacco non-chewing women who cook
regularly with biomass for the past five years or
more showed the prevalence of HTN. Particularly,
compared with those cooks having 5–14 years of
cooking experience (25.4%), HTN was more prevalent
in women cooking for 15 years or more (34.2%) with
biomass, although the difference was not found to
be significant. (30)
Associations
between short term exposure to HAP and BP: Eight
articles investigated the short-term effect of HAP
on BP values. Young et al. assessed exposure to
household air pollution by stove type categories
among 147 women in Honduras. After controlling for
confounders, women using traditional stoves were
nearly twice as likely as women using Justa
stoves to have prevalent borderline high or high
blood pressure. (16)
Similarly, in a
cross-sectional study conducted in three rural
communities in Southern Nigeria, the mean SBP
among biomass fuel users was 135.3 mmHg compared
to 123.8 mmHg among non-biomass fuel users. The
mean DBP among biomass fuel users was 83.7 mmHg,
compared to 80.1 mmHg among non-biomass fuel
users. These differences were statistically
significant. (17) Correspondingly, results of
another intervention study showed that improved
stove intervention was associated with 3.7 mmHg
lower SBP and 3.0 mmHg lower DBP compared with
controls. (24)
In the study by Pena
MB et al., both SBP and DBP were higher by 3.0 and
2.5 mmHg between participants with and without
daily biomass fuel use, respectively. Further, the
authors found an association between biomass fuel
use and both prehypertension and HTN. (22)
Years of
Cooking: Findings from a few studies
indicate that the duration of exposure to biomass
fuels for cooking is an important determinant
factor in the deterioration of pulmonary and
cardiovascular parameters. Yan et al. measured the
solid fuel-related IAP by the years of solid fuel
use. The duration of household solid fuel use was
classified as zero, fifteen, or more than five
years, and the results revealed that users with
the longest duration of solid fuel exposure had
1.63% higher SBP, 1.31% higher DBP, and a higher
risk of HTN with an odds ratio (OR) of 1.55 than
non-users. (22)
Similarly, in
another study conducted in China, Lee et al. found
that, compared with individuals in the lowest
tertile of the duration of solid fuel exposure
(<10 years of use), those in the highest
tertile of the duration of solid fuel exposure
(>25 years of use) had increased odds of HTN.
(20) A similar finding also emanated from a
cross-sectional study carried out in Bangladesh,
which demonstrated that every 1-year increase in
cumulative exposure to biomass smoke eventually
exacerbated the risk of HTN by 61%. (35)
Age: The
rise in BP with age increases the risk of
cardiovascular and renal disease, stroke, and type
2 diabetes mellitus. (44) Even a
reduction of as little as two mmHg in SBP could
lead to 10% lower stroke mortality and 7% lower
mortality from ischemic heart disease or other
vascular causes in middle age. (45)
According to the
study carried out in rural Honduras, the
researchers presented evidence that age impacted
the associations with continuous SBP, with
stronger associations among women who were 40
years of age or older in comparison to women who
were younger.(16)
Similarly, the use
of biogas was associated with 68% reduced odds of
developing HTN in elderly women; however, these
effects were not identified in younger women aged
30–50 years. (19)
Lee et al.'s study
on the Chinese population also revealed that the
association between solid fuel use and risk of HTN
was significant among the ≥ 40-year-old group
compared to the < 40-year-old group. (20)
Likewise, SBP
progressively increased with age in this
population, as reported by Baumgartner et al.,
2011. Among women > 50 years of age, a
1-log-µg/m3 increase in PM2.5
exposure was associated with 4.1 mmHg higher SBP
and 1.8 mmHg higher DBP. Although PM2.5
exposure was positively associated with SBP among
younger women, the association was not
statistically significant.(23)
A considerable
positive association was discovered between the
age of biomass-using women and SBP and DBP,
according to research by Dutta et al. (30, 31).
Alexander et al. observed a statistically
significant decrease in SBP in women >50 years
of age (n=15) 1-year post-intervention, but no
significant decrease was seen in women <50
years of age. (39)
In line with the
above findings, the study in Albania also showed a
significant association between HAP and HTN risk,
especially among participants aged 25 to 54 years
old than among those aged 15 to 24 years old.(36)
On the other hand, a
considerably greater but non-significant pooled
effect on SBP was seen among women above the
median age of 30 compared to those younger in the
multi-country analysis by Arku et al. Although
slightly higher, the odds of HTN in older women
(≥30 years) did not differ significantly from
those in younger (<30 years) women. Similarly,
no statistically significant (pooled) interactions
between age and solid fuel on BP parameters or
odds of HTN were observed.(18)
Effects on
either SBP or DBP: In general, an
individual's "blood pressure" refers to the
pressure measured within large arteries in the
systemic circulation. SBP refers to the maximum
pressure within the large arteries when the heart
muscle contracts to propel blood through the body.
DBP describes the lowest pressure within the large
arteries during heart muscle relaxation between
beating.(45)
While the majority
of research linked using biomass fuels to
increases in both SBP and DBP, the results of the
study by Norris et al. suggest that for rural
Indian women using biomass fuels, increases in
exposure to BC (about a 100 g/m3 increase) are
associated with modest increases only on SBP. (27)
On the contrary, in
an intervention study conducted on pregnant
Nigerian women, the intervention cookstoves showed
the potential to reduce DBP; however, no
significant effect was observed on SBP.(40)
Negative
Association: Of the 28 study articles,
four studies reported a negative association
between using biomass for cooking and either SBP,
DBP, or HTN.
After adjustment for
potential confounders, a cross-section study
conducted in rural Pakistan found no association
of HTN with the use of biomass for cooking in
current users. Also, no associations were apparent
in long-term (≥10 years) users and non-users of
biomass fuel. Further, this study found no
association between the use of biomass fuel and
any of the four outcomes studied (hypertension,
angina, previous history of heart attack and
definite or probable coronary heart disease (CHD)
on electrocardiogram (ECG)), even when the
comparison was with women who had not used biomass
for at least the last ten years.(14)
Similarly, Ofori et
al. found a negative association between HAP and
HTN. (17) A study performed on
pregnant women from central East India also
observed a lower risk of maternal HTN associated
with the use of wood as cooking fuel.(29) In a
large international multi-centre study by Arku et
al., chronic exposure to outdoor PM2.5
was associated with increased BP and HTN but a
small inverse association with HAP. The
researchers observed a decrease in odds of HTN and
a decrease in SBP and DBP among solid fuel users,
but these associations varied notably by study
country and study centre, with generally positive
associations for SBP in China and negative
associations in India and in other countries.(18)
Discussion
Burning biomass
fuels has remained a primary energy source in many
LMICs despite global breakthroughs in the supply
of renewable and sustainable energy. (42)
The impact of HAP on
BP has been the subject of quite a few
meta-analysis and review articles. In the
meta-analysis by Liang et al., each increase in PM2.5
concentration by 10µg/m3 caused
a rise in SBP and DBP but long term exposure
showed the strongest associations. (46)
One recent
meta-analysis, indicated that both short-term and
long-term exposure to some air pollutants might
increase BP values among children and
adolescents.(48)
The literature
review by Giorgini et al., revealed that ambient
and personal exposure to particulate pollution
causes a significant increase in BP. The authors
proposed that although consistent data examining
both PM10 and PM2.5 effects
exist, future evaluations exploring the impact on
BP of personal and mixed air pollution exposure
are needed.(13)
These narrative and
systematic reviews offered proof that air
pollution affects BP, but they were carried out
more than three years ago. A thorough assessment
of the existing literature was necessary because
research on the usage of biomass fuel and its
effects on health has been growing in recent
years. In order to evaluate the data on the
effects of HAP on cardiovascular health through
its impact on BP, this review set out to address
this question.
Our review reveals
that there is a small but growing body of
literature on the connection between BP and HAP
from solid fuel or biomass. Additionally, there is
a lack of consistency in the evidence supporting
the claimed link, with some research showing a
strong association while others show no
association. Further, confounding is an important
potential limitation of several studies because
sex, age, tobacco use, duration of fuel use,
ventilated v. non-ventilated rooms and adoption
and socioeconomic status, all these factors are
associated with several cardiovascular risk
factors, including BP.
To the best of our
knowledge, we have presented a thorough analysis
of practically all research studies that have
investigated an association between at least one
component of IAP or HAP and BP, which is a notable
strength of our review article. Furthermore, we
used three significant databases and a human
search of each selected article's bibliography as
part of our thorough search approach.
Unfortunately, due to a lack of data, we were
unable to address all of the confounding factors,
including sex, socioeconomic position, sample
size, and others, despite our careful and
attentive efforts. Additionally, given limitations
on the clinical perspective of this review, we
have not included studies done in children or
adolescent populations. Additionally, the
definition of HTN differed from article to
article, making the reliability of evidence
pointing to a significant connection questionable.
Additionally, because the concentrations of air
pollution were measured differently in each study,
there may have been some degree of exposure
misclassification. Finally, since our search was
limited to works written in English, it's likely
that pertinent research written in other languages
went undiscovered.
Conclusion
To conclude, the
data imply that even brief exposure to
contaminated air, particularly in the enclosed
setting of the kitchen, might increase blood
pressure, thus increasing the risk of
cardiovascular disease. Despite the fact that some
studies found that the increase in blood pressure
caused by HAP was not statistically significant,
such a little increase may nevertheless be enough
to precipitate a heart attack or stroke in people
who are predisposed to such cardiovascular
disorders. Therefore, it is essential to lower HAP
from solid fuel, which remains one of the main
sources of energy for many families in LMICs.
Hence, until everyone has access to cleaner fuels,
additional efforts should be made to promote the
use of cleaner cooking fuels like LPG in order to
limit exposure to solid fuel smoke.
Additionally, the
conflicting results, as discussed in this review
article, highlight the need for additional
research studies that precisely examine the
relationship between the usage of solid fuel and
preventable cardiovascular risk factors including
blood pressure.
Acknowledgement
The authors would like to thank Dr. Laila Garda,
Director Research, KEM Hospital Research Centre,
Pune, India for her constant guidance and support.
Sources of Funding
This research received no specific grant from
funding agencies in the public, commercial, or
not-for-profit sectors.
References
- Air Pollution [Internet]. World Health
Organization. Available at:
https://www.who.int/health-topics/air-pollution#tab=tab_1
WHO. Air Pollution – Overview and Impacts; 2022.
Accessed March 17th, 2022.
- Cohen A, Brauer M, Burnett R, Anderson H,
Frostad J, Estep K et al. Estimates and 25-year
trends of the global burden of disease
attributable to ambient air pollution: an
analysis of data from the Global Burden of
Diseases Study 2015. The Lancet. 2017
Apr;389:1907-18.
- Kankaria A, Nongkynrih B, Gupta SK. Indoor air
pollution in India: Implications on health and
its control. Indian J Community Med.
2014 Oct-Dec;39:203‑7.
- WHO. WHO publishes new global data on the use
of clean and polluting fuels for cooking by fuel
type [Internet]. World Health Organization.
Available at: https://www.who.int/news/item/20-01-2022-who-publishes-new-global-data-on-the-use-of-clean-and-polluting-fuels-for-cooking-by-fuel-type;
2022. Accessed March 25th, 2022.
- Household air pollution and health [Internet].
World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health;
2022. Accessed May 14th 2022.
- Chakraborty D, Mondal N, Datta J. Indoor
pollution from solid biomass fuel and rural
health damage: A micro-environmental study in
rural area of Burdwan, West Bengal. Int J
Sustain Built Environ. 2014
Dec;3(2):262-71.
- McCracken J, Wellenius G, Bloomfield G, Brook
R, Tolunay H, Dockery D et al. Household Air
Pollution from Solid Fuel Use: Evidence for
Links to CVD. Glob Heart. 2012
Sep;7(3):223-34.
- Indoor Air Quality [Internet] Available at: https://www.epa.gov/report-environment/indoor-air-quality.
Accessed May 14th 2022.
- Nemmar A, Hoet P, Vanquickenborne B, Dinsdale
D, Thomeer M, Hoylaerts M et al. Passage of
Inhaled Particles into the Blood Circulation in
Humans. Circulation. 2002
Jan;105(4):411-4.
- Lim S, Vos T, Flaxman A, Danaei G, Shibuya K,
Adair-Rohani H et al. A comparative risk
assessment of burden of disease and injury
attributable to 67 risk factors and risk factor
clusters in 21 regions, 1990–2010: a systematic
analysis for the Global Burden of Disease Study
2010. The Lancet. 2012
Dec;380(9859):2224-60.
- Fuchs F, Whelton P. High Blood Pressure and
Cardiovascular Disease. Hypertension
2020 Dec;75(2):285-92.
- Fullerton D, Bruce N, Gordon S. Indoor air
pollution from biomass fuel smoke is a major
health concern in the developing world. Trans
R Soc Trop Med Hyg. 2008
Sep;102(9):843-51.
- Giorgini P, Di Giosia P, Grassi D, Rubenfire
M, D. Brook R, Ferri C. Air Pollution Exposure
and Blood Pressure: An Updated Review of the
Literature. Curr Pharm Des.
2016;22(1):28-51.
- Fatmi Z, Coggon D. Coronary heart disease and
household air pollution from use of solid fuel:
a systematic review. Br Med Bull. 2016
Jun;118(1):91–109.
- Das S, Mohapatra I, Samantaray S. Health
impact on women using solid cooking fuels in
rural area of Cuttack district, Odisha. J
Family Med Prim Care. 2018
Jan-Feb;7(1):11-15.
- Young B, Clark M, Rajkumar S, Benka‐Coker M,
Bachand A, Brook R et al. Exposure to household
air pollution from biomass cookstoves and blood
pressure among women in rural Honduras: A
cross‐sectional study. Indoor Air.
2019 Jan;29(1):130-142.
- Ofori S, Fobil J, Odia O. Household biomass
fuel use, blood pressure and carotid intima
media thickness; a cross sectional study of
rural dwelling women in Southern Nigeria. Environ
Pollut. 2018 Nov; 242(Pt A):390-97.
- Arku R, Ezzati M, Baumgartner J, Fink G, Zhou
B, Hystad P et al. Elevated blood pressure and
household solid fuel use in premenopausal women:
Analysis of 12 Demographic and Health Surveys
(DHS) from 10 countries. Environ Res.
2018 Jan;160:499-505.
- Neupane M, Basnyat B, Fischer R, Froeschl G,
Wolbers M, Rehfuess E. Sustained use of biogas
fuel and blood pressure among women in rural
Nepal. Environ Res. 2015
Jan;136:343-51.
- Lee M, Hang J, Zhang F, Dai H, Su L,
Christiani D. In-home solid fuel use and
cardiovascular disease: a cross-sectional
analysis of the Shanghai Putuo study. Environ
Health. 2012 Mar 28;11:18.
- Yan Z, Liu Y, Yin Q, Qiu M. Impact of
household solid fuel use on blood pressure and
hypertension among adults in China. Air
Qual Atmos Health 2016 Feb;9(8):931-40.
- Burroughs Peña M, Romero K, Velazquez E,
Davila-Roman V, Gilman R, Wise R et al.
Relationship Between Daily Exposure to Biomass
Fuel Smoke and Blood Pressure in High-Altitude
Peru. Hypertension. 2015
May;65(5):1134-40.
- Baumgartner J, Schauer J, Ezzati M, Lu L,
Cheng C, Patz J et al. Indoor Air Pollution and
Blood Pressure in Adult Women Living in Rural
China. Environ Health Perspect. 2011
Oct;119(10):1390-5.
- McCracken J, Smith K, Díaz A, Mittleman M,
Schwartz J. Chimney Stove Intervention to Reduce
Long-term Wood Smoke Exposure Lowers Blood
Pressure among Guatemalan Women. Environ
Health Perspect. 2007
Jul;115(7):996–1001.
- Clark M, Bazemore H, Reynolds S, Heiderscheidt
J, Conway S, Bachand A et al. A Baseline
Evaluation of Traditional Cook Stove Smoke
Exposures and Indicators of Cardiovascular and
Respiratory Health among Nicaraguan Women. Int
J Occup Environ Health. 2011
Apr-Jun;17(2):113-21.
- Aung T, Baumgartner J, Jain G, Sethuraman K,
Reynolds C, Marshall J et al. Effect on blood
pressure and eye health symptoms in a
climate-financed randomized cookstove
intervention study in rural India. Environ
Res. 2018 Oct;166:658-667.
- Norris C, Goldberg M, Marshall J, Valois M,
Pradeep T, Narayanswamy M et al. A panel study
of the acute effects of personal exposure to
household air pollution on ambulatory blood
pressure in rural Indian women. Environ
Res. 2016 May;147:331-42.
- Chakraborty D, Mondal N. Hypertensive and
toxicological health risk among women exposed to
biomass smoke: A rural Indian scenario. Ecotoxicol
Environ Saf. 2018 Oct;161:706-714.
- Wylie B, Singh M, Coull B, Quinn A,
Yeboah-Antwi K, Sabin L et al. Association
between wood cooking fuel and maternal
hypertension at delivery in central East India.
Hypertens Pregnancy. 2015; 34(3):
355-68.
- Dutta A, Mukherjee B, Das D, Banerjee A, Ray
M. Hypertension with elevated levels of oxidized
low-density lipoprotein and anticardiolipin
antibody in the circulation of premenopausal
Indian women chronically exposed to biomass
smoke during cooking. Indoor Air. 2010
Apr;21(2):165-76.
- Dutta A, Ray M, Banerjee A. Systemic
inflammatory changes and increased oxidative
stress in rural Indian women cooking with
biomass fuels. Toxicol Appl Pharmacol.
2012 Jun;261(3):255-62.
- Ray M, Mukherjee S, Roychoudhury S,
Bhattacharya P, Banerjee M, Siddique S et al.
Platelet activation, upregulation of CD11b/CD18
expression on leukocytes and increase in
circulating leukocyte-platelet aggregates in
Indian women chronically exposed to biomass
smoke. Hum Exp Toxicol. 2006
Nov;25(11):627-35.
- Dutta A, Ray M. Hypertension and respiratory
health in biomass smoke-exposed premenopausal
Indian women. Air Qual Atmos Health.
2013 Dec;7(2):229-38.
- Arku R, Brauer M, Ahmed S, AlHabib K, Avezum
Á, Bo J et al. Long-term exposure to outdoor and
household air pollution and blood pressure in
the Prospective Urban and Rural Epidemiological
(PURE) study. Environ Pollut. 2020
Jul; 262:114-97.
- Barman N, Haque M, Rahman A, Khalequzzaman M,
Mashreky S. Association of biomass fuel smoke
exposure and hypertension among rural women of
Bangladesh: A cross-sectional study. Indian
J Public Health. 2019
Jul-Sep;63(3):258-260.
- Abba M, Nduka C, Anjorin S, Uthman O.
Household Air Pollution and High Blood Pressure:
A Secondary Analysis of the 2016 Albania
Demographic Health and Survey Dataset. Int J
Environ Res Public Health 2022; 19(5): 2611.
- Quinn A, Ae-Ngibise K, Kinney P, Kaali S,
Wylie B, Boamah E et al. Ambulatory monitoring
demonstrates an acute association between
cookstove-related carbon monoxide and blood
pressure in a Ghanaian cohort. Environ
Health. 2017 Jul 21;16(1):76.
- Clark S, Schmidt A, Carter E, Schauer J, Yang
X, Ezzati M et al. Longitudinal evaluation of a
household energy package on blood pressure,
central hemodynamics, and arterial stiffness in
China. Environ Res. 2019
Oct;177:108592.
- Alexander D, Larson T, Bolton S, Vedal S.
Systolic blood pressure changes in indigenous
Bolivian women associated with an improved
cookstove intervention. Air Qual Atmos
Health. 2014 May;8(1):47-53.
- Alexander D, Northcross A, Wilson N, Dutta A,
Pandya R, Ibigbami T et al. Randomized
controlled ethanol cookstove intervention and
blood pressure in pregnant Nigerian women. Am
J Respir Crit Care Med. 2017
Jun;195(12):1629-39.
- Bond T, Doherty S, Fahey D, Forster P,
Berntsen T, DeAngelo B et al. Bounding the role
of black carbon in the climate system: A
scientific assessment. J Geophys Res Atmos.
2013 Jun;118(11):5380-552.
- Miele C, Checkley W. Clean Fuels to Reduce
Household Air Pollution and Improve Health.
Still Hoping to Answer Why and How. Am J
Respir Crit Care Med. 2017 Jun;
195(12):1552-4.
- Gurven M, Blackwell A, Rodríguez D, Stieglitz
J, Kaplan H. Does Blood Pressure Inevitably Rise
With Age? Hypertension 2012
Jul;60(1):25-33.
- Age-specific relevance of usual blood pressure
to vascular mortality: a meta-analysis of
individual data for one million adults in 61
prospective studies. The Lancet 2002
Dec; 360(9349):1903-13.
- Kovell L, Ahmed H, Misra S, Whelton S,
Prokopowicz G, Blumenthal R et al. US
Hypertension Management Guidelines: A Review of
the Recent Past and Recommendations for the
Future. J Am Heart Assoc. 2015
Dec;4(12):e002315.
- Liang R, Zhang B, Zhao X, Ruan Y, Lian H, Fan
Z. Effect of exposure to PM2.5 on blood
pressure. J Hypertens. 2014
Nov;32(11):2130-41.
- Wu S, Deng F, Huang J, Wang H, Shima M, Wang X
et al. Blood Pressure Changes and Chemical
Constituents of Particulate Air Pollution:
Results from the Healthy Volunteer Natural
Relocation (HVNR) Study. Environ Health
Perspect. 2013 Jan; 121(1):66-72.
- Huang M, Chen J, Yang Y, Yuan H, Huang Z, Lu
Y. Effects of Ambient Air Pollution on Blood
Pressure Among Children and Adolescents: A
Systematic Review and Meta‐Analysis. J Am
Heart Assoc. 2021 May;10(10):e017734.
|



















