|
Introduction:
Breast
lesions in women usually call for medical
attention. Most of the breast lesions are benign,
albeit currently, breast is the leading site of
cancer and cancer related mortality throughout the
world and now in India. [1,2] Early and accurate
diagnosis of these lesions is critical for
selecting appropriate treatment and predicting
treatment outcome.
Breast lesions
encompass a myriad of morphological entities
ranging from non neoplastic, benign to malignant
lesions. The standard triple approach for managing
patients with breast lump include clinical
examination, mammography and biopsy. Despite tru
cut biopsy being considered as an integral part of
triple test, its utility is limited in resource
poor settings. Breast fine needle aspiration
cytology (FNAC) has a long history of providing
accurate, rapid and cost-effective diagnosis of
palpable breast lesions. In resource limited set
ups, FNAC still has a major role to play in
treatment decisions. [3] Similarly, over recent
years, tru cut biopsy has been replaced by FNAC
taking into consideration, the feasibility and
simplicity of the test. [4,5]
Recently,
International Academy of Cytology (IAC) at
Yokohama proposed a new reporting system for
breast cytology, in order to bring uniformity
across the globe.[6] Any new classification system
needs to be validated for its practical
applicability.
The present study
was conducted with the objective to categorize the
breast lesions as per this classification and to
determine the risk of malignancy in each category
as well as the diagnostic efficacy.
Materials and Methods:
The present study
was a cross sectional observational analytical
study conducted over a duration of two years from
January 2020 up to December 2022 in the department
of Pathology, Adichunchanagiri Institute of
Medical Sciences, BG Nagara, Mandya, Karnataka.
Institutional Ethics Committee clearance was
obtained. Sampling method adopted was convenient
sampling, All consecutive cases presenting with
breast lesions in whom FNAC was done in
cytopathology during the study period were
included in the study. Cases with history of
recurrent malignancy, or on
chemotherapy/radiotherapy were excluded from the
study. Sample size was 296. Demographic details
related to each case like age, gender, clinical
history, past history, treatment history if any,
ultrasound findings if available were obtained
from the case records. All 296 FNAC cases were
reclassified according to the newly proposed IAC
Yokohama reporting system. Histologic samples were
considered the gold standard and were available in
88 cases (21.4%).
Statistical analysis:
Statistical analysis
was executed using Microsoft Excel 2011. Standard
descriptive analysis was performed. Sensitivity,
specificity, positive predictive value (PPV),
negative predictive value (NPV) and accuracy
ratios were calculated. The risk of malignancy
(ROM) was defined for each category as the number
of confirmed malignant cases /total number of
cases in each diagnostic category. All the
suspicious and malignant cases were considered as
positive for malignancy. The cases with
insufficient material were excluded from
statistical analysis.
Results
FNAC of 296 cases
were reviewed. Mean age of the patients in the
present study was 44 ± 3.2 years. All the cases
were females except one being male, with female to
male ratio of 20:1. More number of cases presented
with lesion in the right breast with a ratio of
left to right sided lesion being 1: 2.09. All the
cases were unifocal at presentation.
The distribution of
cases in individual cytodiagnostic categories as
described by Yokohama et al is shown in Table 1.
Insufficient material was obtained in 13/296
(4.39%) cases. Benign category included 196/296
(66.21%) cases. 31/296 (10.47%) cases were
categorized as atypia. The suspicious category
included 4/296 (10.47%) cases, while malignant
category included 52/296 (17.56%) cases. In the
suspicious category, suspicious for low grade
malignancy and suspicious for epithelial
malignancy were the diagnosis rendered in 0.67%
cases respectively. In malignant category,
invasive ductal carcinoma-not otherwise specified
was diagnosed in 6.75% cases and ductal carcinoma
in 10.81% cases.
|
Table 1: Shows distribution of
cases in individual cytodiagnostic
categories as described by IAC Yokohoma
system
|
|
Cytodiagnostic categories
|
N
|
Percentage
|
|
Insufficient
|
13
|
4.39%
|
|
Benign
|
196
|
66.21%
|
|
Acute Mastitis
|
20
|
6.75%
|
|
Granulomatous Mastitis
|
7
|
3.57%
|
|
Chronic Mastitis
|
2
|
1.02%
|
|
Galactocele
|
1
|
0.5%
|
|
Fibrocystic change
|
31
|
15.81%
|
|
Lactational change
|
6
|
3.06%
|
|
Normal breast
|
2
|
1.02%
|
|
Atypia
|
31
|
10.47%
|
|
Suspicious
|
04
|
1.35%
|
|
Malignancy
|
52
|
17.56%
|
|
Total
|
296
|
100%
|
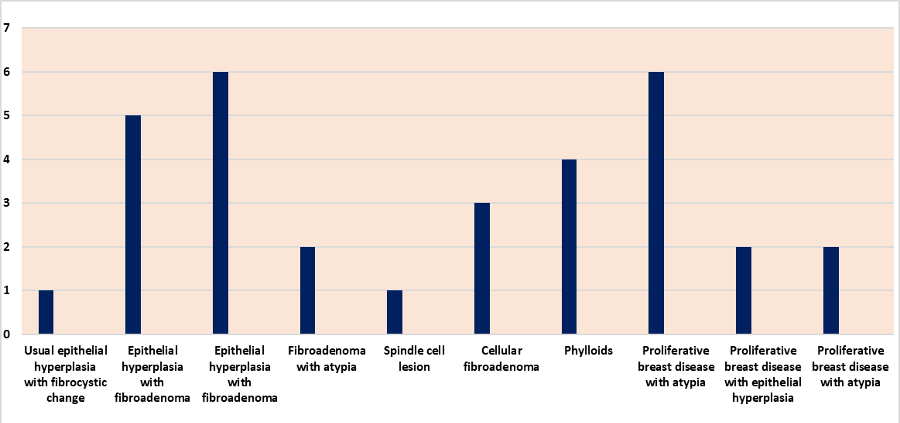
Among 31 cases
included under atypical category, maximum cases
were diagnosed as proliferative breast disease
with atypia (8/31) followed by usual ductal
hyperplasia with fibroadenoma (6/31). Table 2
shows the breakup of cases in category III.
|
Table 2: Showing the distribution
of cases in the category III
|
|
Atypia
|
N
|
|
Usual ductal hyperplasia
|
1
|
|
Usual ductal hyperplasia with fibrocystic
change
|
4
|
|
Usual ductal hyperplasia with
fibroadenoma
|
6
|
|
Fibroadenoma with atypia
|
2
|
|
Spindle cell lesion
|
1
|
|
Cellular fibroadenoma
|
3
|
|
Phylloides tumor
|
4
|
|
Proliferative breast disease with atypia
|
8
|
|
Proliferative breast disease with
epithelial hyperplasia
|
2
|
|
Total
|
31
|
|
| Graph
1: Showing the distribution of cases in
the category III |
Out of total 88
(21.4%) cases for which histopathology was
available, concordance between FNAC and
histopathology diagnosis was obtained in 82
(93.18%) cases, while discordance was noted in
6(6.81%) cases. There were five false negative
(1.66%) and one false positive case (0.33%). Table
3 shows histopathologic correlation among 88
cases. Risk of malignancy in each category is
shown in Table 4. Atypia and suspicious for
malignancy category had ROM of 71.4% and 100%
while in malignant category ROM was 96.66%.
|
Table 3: Cytohistopathology
correlation in 88 cases
|
|
Category
|
FNAC
|
Histopathology
|
|
Concordant
|
Discordant
|
|
Benign (n-50)
|
|
|
|
|
Fibroadenoma
|
30
|
30
|
|
|
Fibrocystic change
|
15
|
15
|
|
|
Mastitis
|
5
|
5
|
|
|
Atypia (n-07)
|
|
|
|
|
Borderline Phylloides
|
2
|
1
|
|
|
Benign fibrous histiocytoma
|
1
|
1
|
|
|
Proliferative breast disease with atypia
|
3
|
|
3
|
|
Phylloides tumor
|
1
|
|
2
|
|
Suspicious (n-02)
|
2
|
2
|
|
|
Malignancy (n-29)
|
29
|
28
|
1
|
|
Total
|
88
|
82
|
6
|
Sensitivity,
specificity, positive predictive value, negative
predictive value and diagnostic accuracy was found
to be 85.71%, 98.11%, 96.55%, 91.23% and 93.02%
respectively.
|
Table 4: Risk of malignancy in
individual category
|
|
Cytodiagnostic category
|
Risk of malignancy
|
|
Insufficient
|
-
|
|
Benign
|
0.01%
|
|
Atypia
|
100%
|
|
Suspicious
|
100%
|
|
Malignancy
|
96.66%
|
|
ROM -Number of confirmed malignant
cases/total number of cases in diagnostic
category
|
Discussion
In the present
study, we retrospectively classified 296 cases as
per the recent IAC Yokohama system, into the five
categories and determined the ROM for each category.
These categories included insufficient, benign,
atypical, suspicious for malignancy and
malignancy. The category I, insufficient or
inadequate category, included cases wherein the
smears show sparse cellularity or which showed
drying artifact or hemorrhage obscuring the
cellular details. In the present study 4.39% cases
had insufficient material. This was in concordance
with the reports of Diana M et al and Sunita H et
al. [7,8] Bajwa R et al reported slightly higher
rate of 13.6% of category I cases. [9] Risk of
malignancy was 0% in this category, in the present
study, similar to that reported by Poornima et al.
[10]
In the present
study, 66.21% of the cases were placed in category
II, i.e, benign, which was in concordance with
that reported by Diana M (73.38%) and Wong S
(72%). [7,11] Maximum number of cases in the
present study were benign, akin to that reported
in literature. [8-11] The most common benign
lesion reported in the present study was
fibroadenoma (28.06%), followed by benign breast
disease (20.40%), fibrocystic change (15.81%),
acute mastitis (6.75%) and granulomatous mastitis
(3.57%). The spectrum of inflammatory lesions
along with lactational changes in shown in Figure
1. Other studies in the literature also observed
fibroadenoma as the most common lesion diagnosed
in this category. In 55 cases of fibroadenoma,
histopathology was obtained and all of these were
concordant with the initial FNA diagnosis. ROM in
this category was 0.01% in the benign category.
Rosa FD et al reported similar ROM for this
category. [12]

|
| Fig
1: Smears show neutrophils in acute
mastitis. (Hematoxylin and Eosin, x 100)
B. Lymphocyte rich smears in chronic
mastitis. (Hematoxylin and Eosin, x 400)
C. Smears show multinucleate giant cells
and epitheloid cells in a mixed
inflammatory background in granulomatous
mastitis. (Hematoxylin and Eosin, x 100)
D. Smear shows foamy histiocytes in a
lipid rich background in lactational
change. Inset shows bare nuclei with
prominent nucleoli (Giemsa, x 100) |

|
| Fig
2: Smears show ductal cells with mild
nuclear atypia in a case of proliferative
breast disease with atypia. (Hematoxylin
and Eosin, x 100) B. Smears show ductal
cells with holes proliferative breast
disease without atypia.(Hematoxylin and
Eosin, x 400) C. Smears show stromal
fragments with high cellularity from a
case of benign phylloides tumor
(Hematoxylin and Eosin, x 100) D. Smear
shows stromal fragments from a case of
benign phylloides tumor showing
characteristic condensation of the nuclei
beneath the peripheral margin (Giemsa, x
100) |
In the present
study, 10.47% cases were placed in category III,
i.e., atypical category. (Figure 2) This was in
accordance with that reported by Rossa FD et al.
[12] The prevalence of atypia show a wide range
across the literature, from 1% to 13%. The
presence of this category which accommodates low
risk indeterminate lesions helps cytopathologists
avoid diagnostic errors by preventing
overdiagnosis in lesions which are predominantly
benign with occasional worrisome features and
reducing false negative diagnosis. [12] In this
category, as shown in graph 1, most common lesions
included showed hyperplasia in the form of three
dimensional overlapping sheets, holes and swirls.
Proliferative disease with atypia were also noted
along with one case of spindle cell lesion. This
spindle cell lesion was a case with a provisional
clinical diagnosis of melanoma, since the lesion
was pigmented. FNAC smears of this lesion showed
short fascicles of uniform spindle cells showing
vague storiform architecture, pigment, touton
giant cells and foamy histiocytes. At FNAC a
diagnosis of benign spindle cell neoplasm,
favouring benign fibrous histiocytoma was made,
which was confirmed by subsequent histopathology.
(Figure 3) ROM in the present study, in atypical
category was 71.4% which was quite high as
compared to that in the literature (20.7% to 38%).
[13] The high ROM in our study could be due to
inclusion of two cases of phylloides tumor in this
category, both of which were malignant at
histopathology.

|
| Fig
3: Smears show spindle cells in short
fascicles cells with mild nuclear
atypia in a case of proliferative breast
disease with atypia. (Hematoxylin and
Eosin, x 100) B. Smears show ductal cells
with holes proliferative breast disease
without atypia.(Hematoxylin and Eosin, x
400) C. Smears show stromal fragments with
high cellularity from a case of benign
phylloides tumor (Hematoxylin and Eosin, x
100) D. Smear shows stromal fragments from
a case of benign phylloides tumor showing
characteristic condensation of the cells
beneath the peripheral margin (Giemsa, x
100) |
In the present
study, suspicious category included 1.35%. which
was similar to that reported by Diana et al, Wong
et al and Panwar et al. [7,11,14] However in
studies conducted by Modi et al, Bajwa et al
Sunita et al and Georgieva et al, authors reported
higher number of cases in this category as 6.5%,
9.3%,6.5% and 5.3% respectively. [15-18] The ROM
in the suspicious category in the present study
was 100%. Similar findings were reported by
Tejaswini et al and Monetzuma et al. [7,19] while
Hoda et al and Wang et al reported a slightly
lower ROM of 85.4% and 84.6% respectively. [11,20]
Malignant category
included 17.56% cases in the present study,
concurrent with that reported in the literature.
ROM in the malignant category in the present study
was 100%, similar to that reported by Panwar et
al, Hoda et al, Montezuma et al and Wang et al
reported a similar ROM of 100%, 98.7%,100% and
99.5% respectively in this category. [7,11,14,20]
Surgery was
performed in total 88 (21.4%) cases in the present
study. Concordance between FNAC and histopathology
diagnosis was obtained in 82 (93.18%) cases, while
discordance was noted in 6 (6.81%) cases. There
were five false negative (1.66%) and one false
positive case (0.33%).
The comparison of sensitivity, specificity,
positive predictive value, and negative predictive
value of the present study with that reported in
the literature, when IAC Yokahama system was
applied is shown in Table 5.
|
Table 5: Comparison of Diagnostic
efficacy of present study with the
existing literature
|
|
Authors
|
Number of cases (FNAC/Histopathology)
|
Sensitivity
|
Specificity
|
PPV
|
NPV
|
Diagnostic accuracy
|
|
De Rose F et al, (2020)
|
4624/1745
|
98.9%
|
46.29%
|
80.5%
|
95%
|
92.82%
|
|
Wong S et al(2019)
|
2696/579
|
83.4%
|
99.4%
|
96.4%
|
97.6%
|
|
|
Agnani B et al
|
603/100
|
88.88%
|
100%
|
100%
|
96%
|
|
|
Sharif A et al
|
100/95
|
91.11%
|
100%
|
100%
|
98.18%
|
|
|
Kamatar P V et al(2019)
|
470/179
|
94.59%
|
98.9%
|
98.59%
|
95.75%
|
96.97%
|
|
Present Study
|
296/88
|
85.71%
|
98.11%
|
96.55%
|
91.23%
|
93.02%
|
|
PPV-Positive predictive value,
NPV-Negative predictive value
|
To conclude, the
high efficacy of FNAC obtained in the present
study, when IAC Yokohama reporting system was
applied, confirms the usefulness of this scheme in
reporting breast lesions. A risk-based
stratification is essential in the present era to
guide and alert the clinician about the subsequent
management plan and the ROM.
References
- WHO. Breast cancer: prevention and control
[Internet]. WHO. [cited 2019 Jul 14]. Available
from:
http://www.who.int/cancer/detection/breastcancer/en/.
- Gupta S. Breast cancer: Indian experience,
data, and evidence. South Asian J Cancer
2016;5:85.
- Pandya AN, Shah NP. Breast fine needle
aspiration cytology reporting: A study of
application of probabilistic approach. Indian
Med Gaz 2013;6.
- Wai CJ, Al-Mubarak G, Homer MJ, Goldkamp A,
Samenfeld-Specht M, Lee Y, et al. A
modified triple test for palpable breast masses:
the value of ultrasound and core needle biopsy.
Ann Surg Oncol 2013;20:850-5.
- Irwig L, Macaskill P, Houssami N. Evidence
relevant to the investigation of breast
symptoms: the triple test. Breast
2002;11:215-20.
- Field AS, Raymond WA, Rickard M, Arnold L,
Brachtel EF, Chaiwun B, et al. The
International Academy of Cytology Yokohama
System for Reporting Breast Fine-Needle
Aspiration Biopsy Cytopathology. Acta Cytol
2019;63:257-73.
- Montezuma D, Malheiros D, Schmitt FC. Breast
Fine Needle Aspiration Biopsy Cytology Using the
Newly Proposed IAC Yokohama System for Reporting
Breast Cytopathology: The Experience of a Single
Institution. Acta Cytol 2019;63:274–79.
- Sunita H, Urmila T, Sharma DC.
Cytomorphological Study Breast Lesions with
Sonomammographic Correlation. Journal of
Evolution of Medical and Dental Sciences 2015;4:14137-42.
- Bajwa R, Tariq Z. Association of fine needle
aspiration cytology with tumor size in palpable
breast lesions. Biomedica 2010;26:124-29
- Kamatar PV, Athanikar VS, Dinesh US. Breast
Fine needle Aspiration Biopsy Cytology Reporting
using International Academy of Cytology Yokohama
System-Two Year Retrospective Study in Tertiary
Care Centre in Southern India. National
Journal of Laboratory Medicine 2019;8:1-3
- Wong S, Rickard M, Earls P, Arnold L, Bako B,
Field AS. The International Academy of Cytology
Yokohama System for reporting breast fine needle
aspiration biopsy cytopathology: A single
institutional retrospective study of the
application of the system categories and the
impact of rapid onsite evaluation. Acta
Cytol 2019;63:280-91.
- Rosa FD,Migliatico I,Vigliar E,Salatiello
M,Pisapia P, Laccarino A, et al. The
continuing role of breast fine-needle aspiration
biopsy after the introduction of the IAC
Yokohama System For Reporting Breast Fine Needle
Aspiration Biopsy. Cytopathology 2020;48:1244-53
- Kocjan G.Fine-needle aspiration cytology.
Inadequate rates compromise success. Cytopathology
2003;14:307-08.
- Panwar H, Ingle P, Santosh T, Singh V, Bugalia
A, Hussain N. FNAC of breast lesions with
special reference to IAC standardized reporting
and comparative study of cytohistological
grading of breast carcinoma. J Cytol 2020;37:34-9.
- Modi P, Haren O, Jignasa B. FNAC as
preoperative diagnostic tool for neoplastic and
non-neoplastic breast lesions: A teaching
hospital experience. Indian J Med Res
2014;4:274-8.
- Bajwa R, Tariq Z. Association of fine needle
aspiration cytology with tumor size in palpable
breast lesions. Biomedica 2010;26:124-9.
- Sunita H, Urmila T, Sharma DC.
Cytomorphological study breast lesions with
sonomammographic correlation. J Evol Med
Dent Sci 2015;4:137-42.
- Georgieva RD, Obdeijn IM, Jager A, Hooning MJ,
Tilanus-Linthorst MM, Van Deurzen CH. Breast
fine-needle aspiration cytology performance in
the high-risk screening population a study of
BRCA1/BRCA2 mutation carrier. Cancer
Cytopathol 2013;121:561-7
- Tejeswini V, Chaitra B, Renuka IV, Laxmi K,
Ramya P, Sowjanya KKS. Effectuation of
International Academy of Cytology Yokahama
Reporting System of Breast Cytology to Assess
Malignancy Risk and Accuracy. J Cytol
2021;38:69-73
- Hoda RS, Brachtel EF. International academy of
cytology Yokohama System for reporting breast
FNAB cytology: A review of predictive values and
risks of malignancy. Acta Cytol
2019;63:292–01.
|



















