|
Introduction:
Drug-induced
hematological disorders can affect all the
hematological elements including red blood cells,
white blood cells, platelets, and the coagulation
system.[1] Drug reaction with eosinophilia and
systemic symptom (DRESS) syndrome is a rare severe
drug-induced idiosyncratic hypersensitivity
response characterized by maculopapular and/or
erythrodermic eruption, fever, peripheral
lymphadenopathy, eosinophilia or atypical
lymphocytosis, and visceral organ involvement. It
usually occurs 2 to 8 weeks after initiating the
offending drug. Of the potential causative agents,
the most common drugs to cause this reaction are
aromatic antiepileptic drugs (especially
phenytoin, carbamazepine, and phenobarbital). The
estimated incidence of this syndrome ranges from
1/1000 to 1/10,000 drug exposures.[2,3]
In this report, we describe a case of DRESS
syndrome in a young female with a unique
presentation.
Case Report
A 22 years female
presented to the OPD with fever, rashes over body
and swelling over face since 1 week. Patient also
experienced difficulty in breathing in the form of
orthopnoea and yellowish discoloration of eyes.
She was suffering from last 2 years with pain and
swelling in different joints and was diagnosed
case of Rheumatoid arthritis. Patient was started
with Sulfasalazine following which after 1 week
patient developed these symptoms. The complete
blood count results revealed hemoglobin level was
11.1 g/dL; platelet count, 296,000/mm3;
and leukocyte count, 55,000 cells per mm3
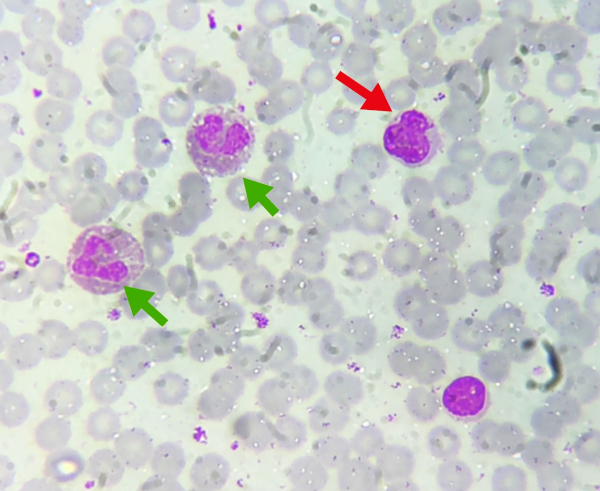
with eosinophilia and lymphocytosis. A peripheral
smear showed atypical lymphocytosis, shift to left
and eosinophilia with absolute eosinophil count of
8,250 cells per mm3 (Fig. 1).
|
|
Figure
1: Peripheral blood smear showing
leucocytosis with atypical lymphocyte
(red arrow) and eosinophils (green
arrows)((Leishman X100).
|
Other investigations
revealed raised serum bilirubin with total
bilirubin level of 2.99 mg/dl, direct was 1.75
mg/dl and indirect was 1.24 mg/dl, mild elevation
of liver transaminases, and lactate dehydrogenase
(aspartate aminotransferase, 64 U/L; alanine
aminotransferase, 168 U/L; lactate dehydrogenase,
625 U/L) were detected. Other biochemistry test
results and coagulation studies were within normal
limits. The chest x ray was normal. She was
hospitalized. Hemoculture, urine culture, and
viral serological tests including hepatitis A, B,
and C, human immunodeficiency virus were all
negative. On further review of the patient’s
history, it was noted that the patient had
received a course of sulfasalazine to treat
rheumatoid arthritis, beginning approximately one
week prior to admission.
The patient's
condition was diagnosed with DRESS syndrome.
Sulfasalazine was stopped. Systemic corticosteroid
(methylprednisolone, 2 mg/kg per day for 7 days)
along with oral antihistamine was initiated. Her
clinical and laboratory findings returned to
normal gradually within the first week of
treatment, and she was discharged with a normal
white blood cell count (10,800 cells per mm3)
and normal differential cell count and absence of
atypical lymphocytes in peripheral blood smear
examination.
Discussion
Various drug induced
hematological syndromes are Immunohemolytic
anemia, Nonimmune hemolytic anemia,
Methhemoglobinemia, Megaloblastic anemia,
Sideroblastic anemia, Aplastic anemia, Pure red
cell aplasia, Immune thrombocytopenia, Thrombotic
microangiopathy, Platelet dysfunction,
Hypercoagulability, Hypoprothrombinemia,
Neutropenia, Neutrophilia, Eosinophilia,
Polycythemia, Acute leukemia/myelodyplasia.[1]
The diagnosis in our
patient was sulfasalazine -induced DRESS syndrome.
Among various diagnostic criteria for DRESS
syndrome, Bocquet et al. were the first to propose
a diagnostic criteria based on the presence of (a)
drug-induced cutaneous eruption, (b) hematological
abnormalities (eosinophilia ≥1.5 × 10[9] /l or
atypical lymphocytes), and (c)systemic
abnormalities which include lymphadenopathy > 2
cm in diameter or hepatitis (transaminases > 2
times the reference value) or interstitial
nephritis or interstitial lung disease, or
myocardial involvement.[4] Various reports are
available of Sulfasalazine-induced DRESS
syndrome.[5]
The diagnosis of
DRESS syndrome can be challenging as it can mimic
many other diseases due to its highly variable
clinical presentation. The differential diagnosis
of this syndrome should include acute viral
infections, hepatitis, sepsis, autoimmune
diseases, and hematologic disorders.[6]
The DRESS syndrome
pathophysiology remains uncertain and is
hypothesized as an immune response to the drug
with expansion of T lymphocytes. In other studies
pathophysiology has been linked to the
reactivation of human herpes virus,
cytomegalovirus and Epstein-Barr virus. Genetic
association is also postulated as it is found that
alleles of the human leukocyte antigen (HLA) have
been associated with increased susceptibility to
DRESS syndrome.[7]
The frequency of
development of DRESS syndrome depends on the drug
used and the immune status of the individual.[2]
The period from drug exposure to onset of disease
can last 2 to 6 weeks, and may persist with a
series of remissions and relapses. After
discontinuation of the drug, the average recovery
time is 6-9 weeks. DRESS syndrome has an
approximate mortality rate of 10%.[2,8,9].
In a retrospective
study conducted by Peyriere et al, among
hematological abnormalities found in 216 cases of
DRESS syndrome, eosinophilia was the most
frequently occurring hematological abnormality
(>50% of the cases). Other hematological
abnormalities observed in patients included
anemia, thrombocytopenia, neutropenia, and the
presence of atypical lymphocytes which were large,
activated lymphocytes.[10]
Silva et al in a
case report found anemia of normocytic
normochromic type, thrombocytopenia, leukocytosis
with mild neutropenia, atypical lymphocytosis and
eosinophilia (AEC- 973/mm3), along with
elevated levels of C-reactive protein (CRP),
transaminases (2 times the reference value),
alkaline phosphatase (ALP), gamma-glutamyl
transpeptidase (GGT), bilirubin (direct and
indirect) and abnormalities in kidney function.[7]
In our case, similar
to study conducted by Peyriere et al and Silva et
al there was eosinophilia and presence of atypical
lymphocytes in peripheral blood additionally there
was leucocytosis and shift to left also and there
were changes in liver function tests also. Our
patient presented with fever and blood cell count
abnormalities which can raise a suspicion for a
hematologic malignancy.
Conclusion
The DRESS syndrome
can be difficult to diagnose as its clinical
findings can mimic those of other systemic
diseases. DRESS should be included in the
differential diagnosis of patients presenting with
fever, rash, and hematological findings as
described above. This case emphasizes the
importance of incorporation of the patient’s
clinical and medication history in the
interpretation of hematological investigations.
Awareness of the clinical, radiologic, and
pathologic findings of DRESS is essential to avoid
a misdiagnosis of hematological malignancy and
hence unnecessary invasive investigations such as
bone marrow examination.
References
- Mintzer DM, Billet SN, Chmielewski L.
Drug-induced hematologic syndromes. Adv
Hematol. 2009;2009:495863. doi:
10.1155/2009/495863.
- Husain Z, Reddy BY, Schwartz RA. DRESS
syndrome: Part I. Clinical perspectives. J
Am Acad Dermatol. 2013;68(5):693.e1-14;
quiz 706-8. doi: 10.1016/j.jaad.2013.01.033.
- Choudhary S, McLeod M, Torchia D, Romanelli P.
Drug Reaction with Eosinophilia and Systemic
Symptoms (DRESS) Syndrome. J Clin Aesthet
Dermatol. 2013;6(6):31-7.
- Bocquet H, Bagot M, Roujeau JC. Drug-induced
pseudolymphoma and drug hypersensitivity
syndrome (Drug Rash with Eosinophilia and
Systemic Symptoms: DRESS). Semin Cutan Med
Surg. 1996;15(4):250-7. doi:
10.1016/s1085-5629(96)80038-1.
- Michel F, Navellou JC, Ferraud D, Toussirot E,
Wendling D. DRESS syndrome in a patient on
sulfasalazine for rheumatoid arthritis. Joint
Bone Spine. 2005;72(1):82-5. doi:
10.1016/j.jbspin.2004.06.002.
- Besli GE, Yildirim S, Yilmaz K, Yuksel E.
DRESS Syndrome or Hematologic Malignancy? A Case
Report of a 4-Year-Old Boy. Pediatr Emerg
Care. 2017;33(7):494-496. doi:
10.1097/PEC.0000000000000489.
- Silva SA, Figueiredo MM, Carneiro L Neto,
Reiss DB, Damásio MA. Drug reaction with
eosinophilia and systemic symptoms (DRESS
syndrome). Rev Assoc Med Bras (1992).
2016;62(3):227-30. doi:
10.1590/1806-9282.62.03.227.
- Cacoub P, Musette P, Descamps V, Meyer O,
Speirs C, Finzi L, et al. The DRESS syndrome: a
literature review. Am J Med. 2011;
124(7):588-97.
- Husain Z, Reddy BY, Schwartz RA. DRESS
syndrome: Part II. Management and therapeutics.
J Am Acad Dermatol. 2013;
68(5):709.e1-9.
- Peyrière H, Dereure O, Breton H, Demoly P,
Cociglio M, Blayac JP, Hillaire-Buys D. Network
of the French Pharmacovigilance Centers.
Variability in the clinical pattern of cutaneous
side-effects of drugs with systemic symptoms:
does a DRESS syndrome really exist? Br J
Dermatol. 2006;155(2):422-8. doi:
10.1111/j.1365-2133.2006.07284.x.
|



















