Introduction:
Over the past few decades, laparoscopic cholecystectomy has solidified
its position as the gold standard for treating symptomatic cholelithiasis.
Due to the development and commitment to the idea of the critical view of
safety, the operation's safety has improved over time. However, the cystic
duct is typically separated closer to the gallbladder to prevent
iatrogenic common bile duct damage when there is severe inflammation in
the triangle of Calot or challenging anatomy, leaving behind a long cystic
duct remnant measuring more than 1 centimeter. This residue may contain
residual calculi or, over time, develop recurrent calculi as a result of
bile stasis, which may result in postcholecystectomy syndrome [PCS] (1-4).
In this context of this, a research study was conducted to assess the
profile of patients treated for PCS due to retained cystic duct stumps.
Material and Methods:
Study Design: Retrospective, cross sectional, descriptive
study.
Data collection and analysis: The study was conducted at
the Department of General Surgery, SKIMS Medical College, Srinagar,
Kashmir. After proper approval from the departmental research and ethics
review committee, a chart review was performed for all the patients
identified as having undergone a surgical reintervention for
postcholecystectomy syndrome due to a retained cystic duct after
laparoscopic cholecystectomy from January 2010 to July 2021. The data
included demographics, details of past surgical operations, clinical
presentation, management, complications, and follow-up.
The exclusion criteria included the cases in which exploration was
undertaken post-cholecystectomy (i) for other complications, including
bile duct injury or bleeding, (ii) for residual gallbladder after
deliberate and documented partial cholecystectomy at the index operation,
and (iii) after index open cholecystectomy.
The data was analysed with Microsoft Excel -2020 and Statistical Package
for the Social Sciences (SPSS v20.0; IBM SPSS, Armonk, NY).
Operative technique: Surgical reintervention for the
residual cystic duct was undertaken under general anaesthesia through a
laparoscopic approach or an open midline or right subcostal incision.
After adhesiolysis, the cystic duct remnant was dissected by approaching
the porta hepatis and the Calot triangle. The dissected duct was clipped
or ligated, leaving a stump less than 1 cm in size. A closed drain was
placed at the end of the procedure.
Results
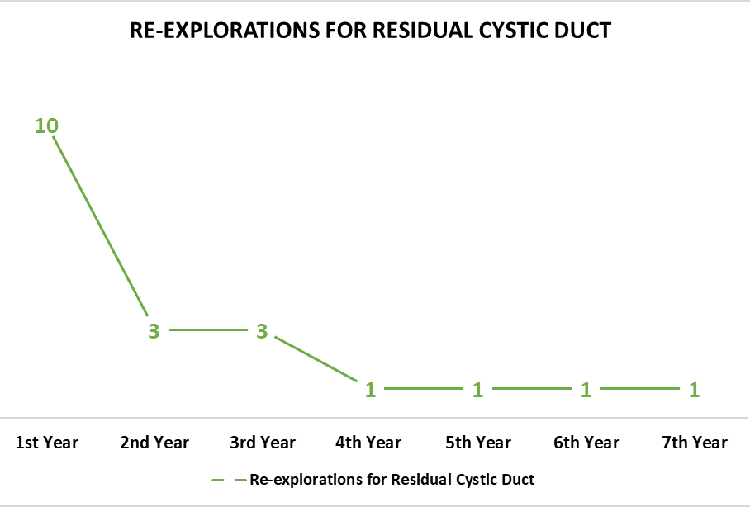
From January 2010 to December 2021, 2176 laparoscopic
cholecystectomies were conducted, and only 20 (0.01%) required
re-exploration for symptomatic residual cystic ducts. As depicted in Table
1, there were 14 males (70%) and 6 females (30%), ranging in age from 21
years to 61 years (mean 33 years and 6 months). The time of presentation
after index cholecystectomy ranged from 3 months to 7 years (mean: 2
years), as depicted in Figure 1, with 10 (50%) presenting within the first
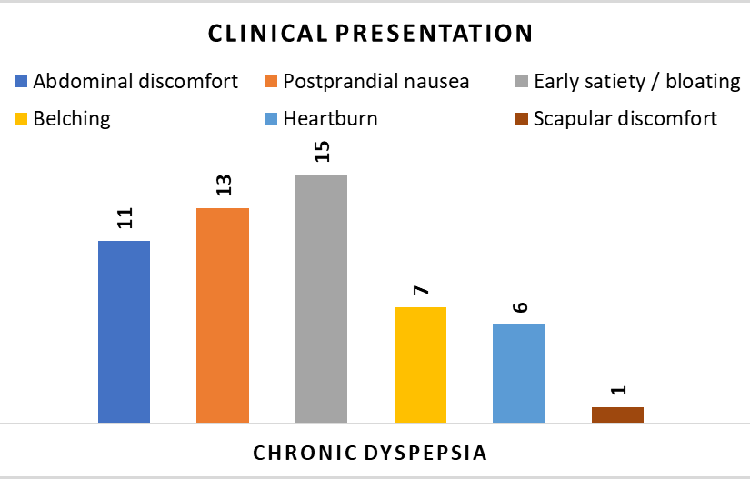
year and 16 (80%) with three years. Seventeen (85%) patients suffered from
chronic dyspepsia (Figure 2), and the symptoms were identified as similar
to their pre-cholecystectomy status in 13 out of these 17 cases (76.5%).
Only three (15%) patients reported an acute abdomen resembling acute
cholecystitis. An abdominal ultrasound (USG) was carried out on all the
patients. An MRI (Magnetic resonance cholangiopancreatography) study and
CT scan were conducted in 7 (35% of the cases) and 6 (30% of the cases,
respectively. All the patients were operated on an elective basis, with
the approach being open in 17 (85%) and laparoscopic in 3 (15%). Cystic
duct remnant had been reported in the operation notes as long in all the
cases, but dimensions were recorded in only 12 cases (range: 2.5 cm-4 cm;
mean 2.8 cm). Cystic duct calculi were found in 5 (25% of the cases),
Hartman's pouch remnants in 2 (10%), and histopathology revealed a neuroma
in 1 (5% of the cases). The approximate operation time ranged from 50 to
120 minutes (mean 87 minutes). The short-term complications included
superficial surgical site infection in 3 (15%) and right basal atelectasis
or pneumonia in 1 (5%). Seven (35%) cases were lost to follow-up, and in the
remaining 13 (65%), the follow-up ranged from 3 months to 3 years (mean: 1
year and 1 month). One (5%) patient reported persistent dyspepsia at
follow-up and was attached to the services of the gastroenterology
division.
|
Table 1: Clinical profile of patients with symptomatic
residual cystic duct.
|
|
S No
|
Gender (M/F)
|
Age (years)
|
Time since index cholecystectomy
(Month - m; year -y)
|
Clinical features
|
Comorbidity, if any
|
Imaging tools used in workup
|
Surgical Approach
|
Stump length (cm)
|
Other findings (Gross /Microscopic)
|
Operation time (minutes)
|
Complications (Yes - Y; No - N; If yes, state)
|
Follow up (months - m; years -y)
|
|
Chronic Dyspepsia
|
Stump cholecystitis (acute)
|
|
USG
|
CT scan
|
MRI
|
Open
|
Laparoscopic
|
|
1
|
M
|
41
|
2y
|
✓
|
|
|
✓
|
|
|
✓
|
|
3
|
|
70
|
N
|
3 y
|
|
2
|
F
|
36
|
3y 6m
|
✓
|
|
|
✓
|
✓
|
|
✓
|
|
2.5
|
CDC
|
85
|
N
|
2y
|
|
3
|
M
|
45
|
8m
|
✓
|
|
|
✓
|
|
|
✓
|
|
-
|
HMR
|
90
|
N
|
-
|
|
4
|
M
|
44
|
6m
|
✓
|
|
|
✓
|
✓
|
|
✓
|
|
2
|
|
70
|
N
|
-
|
|
5
|
F
|
29
|
3y
|
✓
|
|
|
✓
|
|
|
✓
|
|
2.5
|
CDC
|
100
|
Y: SSSI
|
-
|
|
6
|
M
|
38
|
6y
|
✓
|
|
|
✓
|
|
|
✓
|
|
3
|
Neuroma
|
95
|
N
|
1y
|
|
7
|
M
|
41
|
9m
|
✓
|
|
|
✓
|
✓
|
|
✓
|
|
-
|
|
75
|
N
|
-
|
|
8
|
M
|
43
|
2y
|
✓
|
|
|
✓
|
✓
|
|
✓
|
|
3.5
|
HMR, CDC
|
85
|
N
|
-
|
|
9
|
F
|
52
|
2y 6m
|
✓
|
|
DM, HT
|
✓
|
|
|
✓
|
|
-
|
|
120
|
Y: SSSI
|
6m
|
|
10
|
F
|
27
|
9m
|
|
✓
|
|
✓
|
|
|
✓
|
|
2.5
|
|
75
|
N
|
1y
|
|
11
|
M
|
34
|
1y 9m
|
✓
|
|
|
✓
|
✓
|
|
✓
|
|
4
|
|
100
|
N
|
-
|
|
12
|
M
|
45
|
6m
|
✓
|
|
|
✓
|
|
|
✓
|
|
-
|
|
95
|
N
|
6m
|
|
13
|
M
|
56
|
7y
|
✓
|
|
|
✓
|
|
✓
|
✓
|
|
-
|
CDC
|
85
|
N
|
-
|
|
14
|
F
|
61
|
8m
|
|
✓
|
HT
|
✓
|
|
✓
|
✓
|
|
3
|
|
110
|
N
|
2y
|
|
15
|
M
|
44
|
5y
|
✓
|
|
|
✓
|
✓
|
|
|
✓
|
2
|
CDC
|
65
|
N
|
3y
|
|
16
|
F
|
38
|
10m
|
✓
|
|
|
✓
|
|
✓
|
|
✓
|
-
|
|
85
|
Y: basal atelectasis
|
6m
|
|
17
|
M
|
57
|
3y
|
✓
|
|
HT
|
✓
|
|
✓
|
✓
|
|
2.5
|
CDC
|
105
|
Y: SSSI
|
6m
|
|
18
|
F
|
32
|
6m
|
|
✓
|
DM
|
✓
|
|
✓
|
|
✓
|
-
|
|
100
|
N
|
3m
|
|
19
|
M
|
37
|
3m
|
✓
|
|
|
✓
|
|
✓
|
✓
|
|
3
|
|
80
|
N
|
1y
|
|
20
|
M
|
46
|
4m
|
✓
|
|
HT
|
✓
|
|
✓
|
✓
|
|
-
|
|
50
|
N
|
6m
|
|
CDC: Cystic duct calculi; SSSI: Superficial surgical site
infection; HMR: Hartman's pouch remnant
|
|
Figure 1: Time-frame of re-explorations
for symptomatic residual cystic duct.
|
|
Figure 2: Symptoms in patients of residual
cystic duct presenting as chronic dyspepsia.
|
Discussion
In recent decades, laparoscopic cholecystectomy has attained the status
of the gold standard for the treatment of symptomatic cholelithiasis. Some
patients, however, suffer from a complication termed postcholecystectomy
syndrome (PCS), wherein the preoperative symptoms may persist after open
or laparoscopic cholecystectomy (5). In laparoscopic cholecystectomy,
particularly in the presence of acute cholecystitis or distorted anatomy,
there is a tendency to divide the cystic duct closer to the gallbladder to
avoid iatrogenic common bile duct damage, thereby leaving behind a cystic
duct remnant that measures greater than 1 centimeter. This remnant may, in
the course of time, lead to PCS, especially when calculi are present
(6-7). The incidence of PCS varies widely in the literature, from 5 to 30%
(8). As the name implies, this syndrome can either signify the emergence
of new symptoms that are often associated with the gallbladder or the
persistence of symptoms brought on by gallbladder pathology, which include
fatty food intolerance, nausea and vomiting, heartburn, postprandial
fullness, bloating and flatulence, indigestion, and intermittent episodes
of abdominal pain. To arrive at a correct diagnosis, a thorough history,
meticulous physical examination, laboratory work, abdominal imaging,
and/or endoscopy are useful, as they help in identifying or ruling out
either biliary or non-biliary aetiologies of PCS (9).
PCS can present early, typically in the post-operative period, but can
also appear months to years later. PCS may occur secondary to the
gallbladder remnant, a long cystic duct stump, surgical bed scarring or
neuromas, biliary strictures, sphincter of Oddi dysfunction, recurrent
calculi, granulomas, or choledochocele. A high index of suspicion is
needed to diagnose this condition, but as the symptoms are very similar to
those of PCS, they may arise from other organic gastrointestinal
disorders, and the differential diagnosis can be extensive (10).
In our series, the mean time between the primary cholecystectomy and
presentation was 2 years. In the literature, a wide range of time has been
documented. In a recent series by Popescu et al., the period between the
primary surgery and the surgery to complete the resection varied between 2
years and 22 years (11). Palanivelu et al. reported 15 patients with
cystic duct remnant calculi in whom the duration between the index surgery
and re-exploration ranged between 6 months and 10.7 months (12).
In the present series, a transabdominal ultrasound study was conducted in
all the cases as the first-line imaging modality, and a CT scan or MRI was
done as the second-line modality in 7 (35%) and 6 (30%) cases,
respectively. This approach concurs with the findings in the literature.
The accuracy of transabdominal USG in the detection of cystic duct
remnants was found to be 60% by Palanivelu et al.(12) However, this
imaging modality is user-dependent. Filip et al. (13), while prospectively
evaluating 80 patients with postcholecystectomy symptoms, used
transabdominal USG as the first tool but followed with endoscopic
ultrasound (EUS) and found that the sensitivity and specificity of EUS
were high in the subgroup of patients with biliary or pancreatic symptoms
(96.2% and 88.9%) and helped to indicate subsequent investigations like
ERCP. MRCP was found to be similar to EUS in sensitivity and specificity,
besides being non-invasive and posing no radiation risk.
The surgical approach for re-exploration in this series was open in 17
(85%) and laparoscopic in 3 (15%), and all the patients were operated on
an elective basis after proper optimization, including the 3 (15%) that
had reported with acute symptoms. Laparoscopic approach has been adopted
in the last four years. This can be explained on the basis of the learning
curve of the surgeons. The literature from the high-volume centres shows
that the laparoscopic approach can be used very successfully in
re-exploration. Palanivelu et al. in their series managed 15 patients
(100%) with cystic duct remnants by successful laparoscopic excision (12).
Popescu et al., in their series, re-explored 14 (100%) patients
laparoscopically, and there were 4 cases of subtotal cholecystectomies and
10 cases of cystic duct stump stones. They concluded that the laparoscopic
approach is preferable for re-exploration due to the benefits that
laparoscopic surgery brings, but stressed the requirement of surgeons
experienced in advanced laparoscopic techniques because of adhesions
following the previous procedure (11). In a series by Tania et al., all 7
cases were treated laparoscopically without conversion with a mean
operative time of 62 minutes, and the authors stress that despite
adhesions in the gallbladder fossa, these patients can be managed well
with laparoscopic surgery (14). They emphasized the importance of proper
dissection and identification of the gallbladder - cystic duct junction to
minimize the chances of leaving a residual stump. They further emphasized
that the cystic duct stump calculi diagnosed on ultrasound as a cause of
these symptoms may actually be in the remnant gall bladder (14).
Matsudaira et al. in 2020 reported the safe and successful application of
intraoperative near-infrared (NIR) fluorescence cholangiography to
visualize the biliary tract while performing laparoscopic remnant cystic
duct resection (10). For patients unfit for surgery, certain other
treatment modalities are mentioned in the literature, including endoscopic
retrograde cholangiopancreatography with basket (15), laser lithotripsy
(16), and extracorporeal shockwave lithotripsy (ESWL) with or without
endoscopic stone removal.
Conclusion
In the current era of laparoscopic surgery, there is a tendency to leave
behind a longer cystic duct stump due to the practice of ligating the
cystic duct close to the gall bladder to avoid common bile duct injuries,
thereby predisposing to postcholecystectomy syndrome. We should be aware
of this entity and evaluate it for this condition by conducting proper
investigations if no other cause of the symptoms is found. Transabdominal
USG followed by MRCP or endoscopic USG can clinch the diagnosis. Surgery
is the treatment of choice, and a laparoscopic approach in the hands of an
expert surgeon can be adopted safely.
Limitations
The data may not be conclusive, and this possibility arises from the fact
that the patients are not legally bound to follow-up at a particular
treating institution, and hence, there is a potential that some
symptomatic cases may have sought treatment from other healthcare
facilities in the government and private sector. This factor is worth
mentioning because, over the last decade, the healthcare setup has
significantly improved due to the commissioning of multiple tertiary and
secondary healthcare facilities in the Kashmir valley.
Acknowledgments
All authors declare that they have no conflicts of interest. Author 1
(AAR) has compiled the data and results, and the other two authors (SAS
and MAF) have participated in the compilation of the other components of
the article.
References
- Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc. 2002 Jun;16(6):981-4
- Vyas FL, Nayak S, Perakath B, Pradhan NR. Gallbladder remnant and
cystic duct stump calculus as a cause of postcholecystectomy syndrome.
Trop Gastroenterol. 2005 Jul-Sep;26(3):159-60.
- Chatra PS. Cystic duct remnant: a rare cause for post-cholecystectomy
syndrome. BJR Case Rep. 2017 Nov 22;4(1):20170043.
- Mergener K, Clavien PA, Branch MS, Baillie J. A stone in a grossly
dilated cystic duct stump: a rare cause of postcholecystectomy pain. Am
J Gastroenterol. 1999 Jan;94(1):229-31.
- Peterli R, Merki L, Schuppisser JP, Ackermann C, Herzog U, Tondelli P.
Postcholecystectomy complaints one year after laparoscopic
cholecystectomy. Results of a prospective study of 253
patients. Chirurg. 1998 Jan;69(1):55-60.
- Shaw C, O'Hanlon DM, Fenlon HM, McEntee GP. Cystic duct remnant and
the 'post-cholecystectomy syndrome'. Hepatogastroenterology. 2004
Jan-Feb;51(55):36-8.
- Rozsos I, Magyaródi Z, Orbán P. The removal of cystic duct and
gallbladder remnant by microlaparotomy. Acta Chir Hung.
1997;36(1-4):297-8.
- Mohamadnejad M, Hashemi SJ, Zamani F, Baghai-Wadji M, Malekzadeh R,
Eloubeidi MA. Utility of endoscopic ultrasound to diagnose remnant
stones in symptomatic patients after cholecystectomy. Endoscopy. 2014
Aug;46(8):650-5.
- Schofer JM. Biliary causes of postcholecystectomy syndrome. J Emerg
Med. 2010 Oct;39(4):406-10.
- Matsudaira S, Fukumoto T, Yarita A. Hamada J, Hisada M, Fukushima J,
Kawarabayashi N. A patient with cystic duct remnant calculus treated by
laparoscopic surgery combined with near-infrared fluorescence
cholangiography. Surg Case Rep 2020; 6 :146.
- Popescu RC, Leopa N, Dumitru A, Dan C, Dosa A, Bosneagu R, Lordache
IE, Botea F. Residual Gallbladder and Cystic Duct Stump Stone after
Cholecystectomy: Laparoscopic Management. Chirurgia (Bucur). 2021
Aug;116(4):484-491.
- Palanivelu C, Rangarajan M, Jategaonkar PA, Madankumar MV, Anand NV.
Laparoscopic management of remnant cystic duct calculi: a retrospective
study. Ann R Coll Surg Engl. 2009 Jan;91(1):25-9.
- Filip M, Saftoiu A, Popescu C, Gheonea DI, Iordache S, Sandulescu L,
Ciurea T. Postcholecystectomy syndrome - an algorithmic approach. J
Gastrointestin Liver Dis. 2009 Mar;18(1):67-71.
- Tantia O, Jain M, Khanna S, Sen B. Post cholecystectomy syndrome: Role
of cystic duct stump and re-intervention by laparoscopic surgery. J
Minim Access Surg. 2008 Jul;4(3):71-5.
- Pawa R, Dorrell R, Pawa S. Endoscopic management of cystic duct stones
and Mirizzi's syndrome: experience at an academic medical center. Endosc
Int Open. 2022 Jan 14;10(1):E135-E144.
- Benninger J, Rabenstein T, Farnbacher M, Keppler J, Hahn EG, Schneider
HT. Extracorporeal shockwave lithotripsy of gallstones in cystic duct
remnants and Mirizzi syndrome. Gastrointest Endosc. 2004
Sep;60(3):454-9.
|

