Case Report
Xanthogranulomatous Osteomyelitis Masquerading as Neoplasm in a Rare Site
Authors:
Manjula, Second Year Post Graduate Resident, Department of Pathology,
Jayanthi C, Associate Professor, Department of Pathology,
Rajkumar Pandian, Third Year Post Graduate Resident, Department of Orthopaedics,
Naveen Kumar, Assistant Professor, Department of Orthopaedics,
Erli Amel Ivan, Professor and Head of Department of Pathology,
Pragash, Professor and Head of Department of Orthopaedics,
Sri Manakula Vinayagar Medical College and Hospital, Kalvi Vallal N. Kesavan Salai, Kalitheerthalkuppam, Madagadipet,
Puducherry - 605 107
Address for Correspondence
Dr. Jayanthi C,
Associate Professor,
Department of Pathology,
Sri Manakula Vinayagar Medical College and Hospital,
Kalvi Vallal N. Kesavan Salai,
Kalitheerthalkuppam,
Madagadipet,
Puducherry - 605 107, India.
E-mail: drjayanthichandran@gmail.com.
Citation
Manjula, Jayanti C, Pandian R, Kumar N, Ivam EA, Pragash. Xanthogranulomatous Osteomyelitis Masquerading as Neoplasm in a Rare Site. Online J Health Allied Scs.
2021;20(3):18. Available at URL:
https://www.ojhas.org/issue79/2021-3-18.html
Submitted: Aug 20,
2021; Accepted: Oct 1, 2021; Published: Oct 31, 2021 |
|
|
|
Introduction:
Xanthogranulomatous inflammation is a chronic inflammatory process histologically characterised by collection of foamy macrophage admixed with polymorphonuclear leukocytes, activated plasma cell, lymphocyte of polyclonal origin.[1] This condition is mainly encountered in soft tissues and the various tissues which have described it are gall bladder, kidney, lung, gastrointestinal and urogenital tracts.[2] Involvement of brain and bone are infrequent. The distinctive feature of xanthogranulomatous osteomyelitis is the presence of granular, eosinophilic, periodic acid Schiff (PAS) positive histiocytes to start with; followed by collection of mixture of chronic inflammatory immune cells mainly foamy macrophages and activated plasma cells. Gross and radiological examination can mimic malignancy, and discernment is done mainly by histopathological evaluation. We report a case of xanthogranulomatous osteomyelitis which presented as a swelling in the left fourth finger.
Case Report
A 22 year old female presented to the orthopaedics outpatient department with complaints of pain over left fourth finger since 7 months. Pain was insidious in onset, continuous in nature and radiating to left hand. Pain aggravated with lifting heavy objects. There was no history of trauma. On examination the pain score on the left hand was 6/10. Tenderness over fourth proximal phalanx with no swelling or deformity was noted. No bony irregularity or thickening. No scars or discharging sinus over the region. No restrictions of movements.
 |
Fig 1: Plain X Ray of left hand showing eccentric, lytic lesion in the base of 4th proximal phalanx (PPX). |
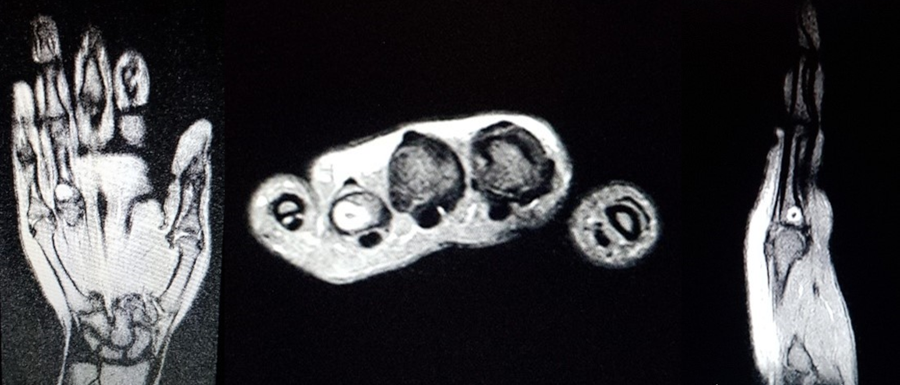 |
Fig 2:
Well defined intramedullary T1 isointense and T2/STIR hyperintense lesion in the proximal phalanx of 4th digit with intralesional calcification. Features suggestive of Enchondroma. |
 |
Fig 3a: Intraoperative image showing curettage of lesion with prepared cavity.
Fig 3b: Yellowish grey marrow material |
 |
 |
Fig 4: Post operative wound with no signs of secondary infection |
Fig 5: Post-operative X ray showing cavity filled with cancellous bone graft material |
 |
 |
Fig 6: Photomicrograph showing sheets of foamy histiocytes admixed with chronic inflammatory cells and sequestrum. (100X; haemotoxylin and eosin stain). |
Fig 7: Photomicrograph showing sheets of foamy histiocytes. (400X; haemotoxylin and eosin stain). |
Plain X ray of left hand AP and lateral views showed eccentric, lytic and non expansile lesion at the base of the 4th PPX. No evidence of periosteal reaction or cortical breach (Fig 1)
Contrast enhanced Magnetic resonance imaging (CEMRI) showed a well defined intramedullary T1 isointense and T2/STIR hyperintense lesion measuring 7 x 8 x 8 mm noted in the proximal phalanx of the fourth digit with intralesional calcification and post contrast enhancement, with a provisional diagnosis of Enchondroma. (Fig 2)
Laboratory investigation showed leucocytosis with neutrophilia, elevated erythrocyte sedimentation rate and C reactive protein suggestive of inflammation. With a provisional diagnosis of Enchondroma, curettage, biopsy and olecranon bone grafting was planned.
Intra operatively extended curettage was done (Fig 3a) and yellowish white marrow particles (Fig 3b) were seen, which were sent for histopathological examination and culture study. Chemical cauterization with hydrogen peroxide solution was done. Cavity scrapped well off debris until active bleeding was evident. Cavity was prepared. Cancellous bone graft taken from ipsilateral olecranon by open door technique and packed in the cavity. Wound was closed in layers. Alternate day dressing was done. Finger mobilization started from post-operative day 2. Wound healing was good. No signs of infection (Fig 4). Sutures were removed on post-operative day 11.
Histopathological examination of the debrided material revealed sheets of foamy histiocytes, lymphocytes, plasma cells, neutrophils and giant cells. Fragments of both viable and dead bone tissue surrounded by dense mixed inflammation along with foci of necrosis were noted (Fig 6 and 7). Special stain using PAS was negative. The tissue cultures failed to reveal any organisms. The postoperative period was uneventful. This case is presented to affirm the importance of histopathological examination to discern the chronic inflammatory process masquerading as neoplasm both on clinical and radiological examination.
Discussion
Xanthogranulomatous osteomyelitis is a notable disease in terms of its rarity. To the best of our knowledge the reported incidence of xanthogranulomatous osteomyelitis is merger. It is a benign and curable disease which can mimic malignant bone tumor both clinically and radiologically. Presenting as a solid mass it is often confounded to be an infiltrative neoplasm both radiologically and grossly. The role of histopathological examination in making a confirmative diagnosis of xanthogranulomatous osteomyelitis has been emphasised in various studies. In our case both X ray and CEMRI finding were suggestive of Enchondroma. At present, there is no concise imaging finding to differentiate this chronic inflammatory condition from neoplastic lesions.
Literature review has failed to define the exact pathogenesis of the above condition. However defective lipid transport, immunological disorders, low virulent infections, reactions to specific infectious agents, and lymphatic obstruction has been proposed as putative mechanisms of origination of xanthogranulomatous osteomyelitis. With respect to the cell of origin, it is considered that majority of foam cells are derived from monocytes/macrophages. Delayed type hypersensitivity reaction of cell mediated immunity has been largely studied to play an immune role in the development of xanthogranulomatous osteomyelitis.[2] Though the obligatory role of bacterial infection in xanthogranulomatous lesions of many organ sites has been established, its role in bone is yet to be confirmed by further studies. A hypothetical relationship between trauma and xanthogranulomatous osteomyelitis developing at the same site has been reported by Solooki et al.[2] But our case has no association with trauma. Evidences in literature have described its incidence in long and flat bones only. However our case is the second one next to Cennimo et al[3] to report it in small bone that is in phalanx ( Table 1).
Xanthogranulomatous osteomyelitis is characterized histologically by abundant foamy histiocytes, multinucleated giant cells, cholesterol clefts and fibrosis together with plasma cells, lymphocytes, and polymorphonuclear cells. The list of histological differential diagnosis of xanthogranulomatous osteomyelitis includes Langerhans cell histiocytoses, Erdheim-Chester disease, chronic recurrent multifocal osteomyelitis, xanthoma, infiltrative storage disorder, malakoplakia, fibrohistiocytic tumor and metastatic renal cell carcinoma.[4] Clinical presentation, radiology, histopathological findings with special stains and ultra structure examination together are important in making a comprehensive diagnosis of xanthogranulomatous osteomyelitis.
| Table 1: Review of previously published cases with Xanthogranulomatous osteomyelitis. |
Site |
Author |
Age/Sex |
Radiological findings |
Clinical diagnosis |
Treatment |
Tibia |
Solooki et al.[2] |
15/M |
Expansile bony lesion. |
Osteomyelitis, Ewings sarcoma, Osteosarcoma. |
IV and Oral antibiotics. |
Femur |
Nalini et al.[5] |
20/F |
Osteolytic lesion. |
|
Curettage with bone grafting. |
Humerus |
Cheema et al.[7] |
5/F |
Multiple osteolytic lesion. |
|
IV and Oral antibiotics. |
Ulna |
Vankalakunti et al.[4] |
50/F |
X Ray - osteolytic lesion. |
Tumor. |
Curettage with bone grafting. |
Rib |
Cozzutto et al.[6] |
5/M |
X Ray - osteolytic lesion. |
Ewings sarcoma, Chronic osteomyelitis. |
En bloc resection of first rib. |
Index Finger And Wrist |
Cennimo et al.[3] |
41/M |
X ray - soft tissue swelling.
MRI - abscess formation. |
Abscess |
Antibiotics and Synovectomy. |
Medial Malleolus, Talus, Cuboid. |
Sapra et al.[8] |
34/M |
Osteolytic lesion |
|
Curettage with bone grafting.
|
Conclusion:
This case is presented for its rarity and to emphasise the importance of histopathological examination of any mass lesion of bone. Being aware of such entity and comprehensive diagnosis on histopathology are crucial in appropriate management of this disease as it's a curable condition.
References:
- Lee SH, Lee YH, Park H, Cho YJ, Song HT, Yang WI, et al. A case report of xanthogranulomatous osteomyelitis of the distal ulna mimicking a malignant neoplasm. Am J Case Rep 2013;14:304-307.
- Solooki S, Hoveidaei AH, Kardeh B, Azarpira N, Salehi E. Xanthogranulomatous Osteomyelitis of the Tibia. Ochsner J 2019;19(3):276-281.
- Cennimo DJ, Agag R, Fleegler E, Lardizabal A, Klein KM, Wenokor C, et al. Mycobacterium marinum Hand Infection in a "Sushi Chef". Eplasty 2009;9:e43.
- Vankalakunti M, Saikia UN, Mathew M, Kang M. Xanthogranulomatous osteomyelitis of ulna mimicking neoplasm. World J Surg Oncol 2007;5:46.
- Nalini G. Xanthogranulomatous osteomyelitis: a case report. Med J 2014;1(6):45-47.
- Cozzutto C. Xanthogranulomatous osteomyelitis. Arch Pathol Lab Med 1984;108(12):973-976.
- Cheema A, Arkader A, Pawel B. Xanthogranulomatous osteomyelitis of the humerus in a pediatric patient with Alagille syndrome: a case report and literature review. Skeletal Radiol 2017;46(10):1447-1452.
- Sapra R, Jain P, Gupta S, Kumar R. Multifocal bilateral xanthogranulomatous osteomyelitis. Indian J Orthop 2015;49(4):482-484.
|

